ALS Isn’t Just About Muscle Weakness - It’s About Breathing and Eating
When someone is diagnosed with ALS, the focus often turns to losing the ability to walk, speak, or hold a spoon. But two silent battles - breathing and eating - are what truly determine how long and how well a person lives. Noninvasive ventilation (NIV) and proper nutrition aren’t optional extras. They’re the two most powerful tools we have to slow decline, reduce suffering, and add months, even years, to life.
Why Breathing Gets Harder in ALS - And How NIV Helps
ALS attacks the nerves that control the diaphragm, the main muscle that pulls air into your lungs. As it weakens, breathing becomes shallow. At first, it’s subtle - waking up with a headache, feeling tired by midday, or needing extra pillows to sleep. These aren’t just annoyances. They’re warning signs your body isn’t getting enough oxygen or is drowning in carbon dioxide.
Noninvasive ventilation steps in with a simple machine: a mask over your nose or mouth, connected to a ventilator that pushes air in when you breathe in and helps it out when you breathe out. Most use bilevel positive airway pressure (BiPAP) - a device that adjusts pressure between inhale and exhale. It doesn’t replace your lungs. It just gives them a boost.
Studies show NIV can add about 7 months to life on average. One 2006 study found people who used NIV lived 453 days longer than those who didn’t. That’s not a guess - it’s measured in real people. And it’s not just about living longer. People report fewer morning headaches, deeper sleep, and more energy during the day. One ALS forum user wrote, “I felt like I could finally breathe again after 3 weeks of using it.”
When to Start NIV - And Why Waiting Can Hurt
Many doctors wait until forced vital capacity (FVC) drops below 50% before recommending NIV. But that’s too late. European and Canadian guidelines say start when FVC falls below 80% or when symptoms like daytime sleepiness or morning headaches appear. The U.S. insurance system often lags behind science - requiring stricter numbers before approving coverage. That creates a dangerous gap.
Don’t wait for your doctor to bring it up. If you’re having trouble sleeping, feeling exhausted by noon, or waking up with a pounding headache, ask about NIV. The American Academy of Neurology says counseling on NIV should happen within 30 days of FVC dropping below 80% or when respiratory symptoms start. And here’s something many don’t know: bulbar weakness (trouble swallowing or speaking) doesn’t make NIV less effective. A 2013 study showed people with bulbar ALS get the same survival benefit as those without it.
NIV Devices: BiPAP vs. Portable Ventilators
Not all machines are the same. Basic BiPAP devices cost $1,200-$2,500 and are meant mostly for nighttime use. They’re good for early-stage ALS. But as the disease progresses, you might need more.
Portable ventilators like the Philips Respironics Trilogy 100 or 106 are heavier, cost $6,000-$10,000, but offer real advantages: they can run on battery for 8-12 hours, support daytime use, and adjust pressure automatically based on your breathing. They include built-in oxygen monitoring and dual backup systems. ALS users who switched to Trilogy report higher satisfaction - 4.2 out of 5 on ALS Toolkit reviews - compared to 3.7 for standard BiPAPs.
Mask comfort matters too. Many people quit because their skin breaks down or the mask feels like a vice. Newer masks are lighter, use softer materials, and come in multiple styles - nasal pillows, full face, hybrid. Don’t settle for the first one you’re given. Work with a respiratory therapist. Try three different masks before deciding.
Adherence Is the Real Challenge - And It’s Surmountable
Using NIV isn’t like taking a pill. You have to wear a mask every night. And many don’t. Early on, only about 20 days out of 30 are used. But here’s the good news: adherence improves dramatically. By one year, most users are wearing it 27-30 days a month.
Why? Support. A 2019 study found patients who got help from respiratory therapists - not just a machine handed to them - were far more likely to stick with it. Therapists adjust pressure settings, fix leaks, teach breathing techniques, and troubleshoot anxiety. One therapist in Austin told me, “I spend 90 minutes with each new patient. That’s not a billable hour - it’s the difference between life and silence.”
Common problems? Mask discomfort (63%), skin sores (41%), and feeling like you can’t exhale (38%). The solution isn’t quitting. It’s tweaking. Lowering EPAP pressure, switching to a different mask, adding humidification, or using a ramp feature that slowly increases pressure as you fall asleep.
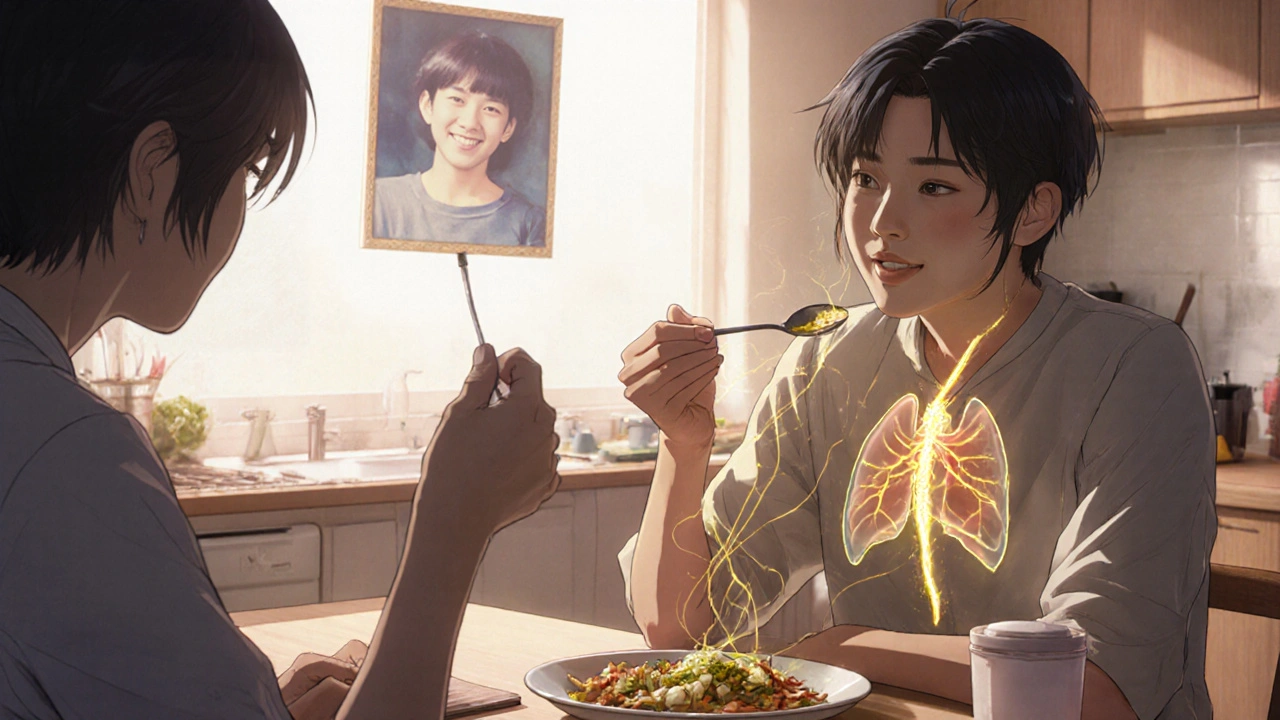
Nutrition Isn’t About Calories - It’s About Timing
Weight loss in ALS isn’t normal. It’s a sign your body is burning through muscle just to stay alive. Losing even 10% of your body weight cuts survival time in half. That’s why nutrition isn’t about fancy diets or protein shakes. It’s about preventing that loss before it starts.
The gold standard is a PEG tube - a feeding tube placed directly into the stomach through a small incision in the abdomen. It’s not a last resort. It’s a preventive tool. The American Academy of Neurology recommends it when weight loss begins or when FVC drops below 50% or BMI falls under 18.5. Why? Because once swallowing becomes dangerous, it’s too late.
A 2006 study showed that without a PEG, ALS patients lost 12.6% of their body weight in six months. With a PEG, weight loss dropped to 0.5%. That’s not a small difference - it’s life-changing. And it adds about 120 days to life.
Many fear the tube means giving up. But it doesn’t. People still eat what they can. The tube just ensures they get enough nutrition when swallowing fails. It’s like a backup generator - you don’t turn on the lights until the power goes out. But with ALS, you install the generator before the storm hits.
How to Know If It’s Time for a PEG
Don’t wait until you’re choking on food or losing weight rapidly. Watch for these signs:
- Taking more than 30 minutes to finish a meal
- Needing to drink water with every bite
- Food sticking in your throat
- Unintentional weight loss over a few weeks
- Aspiration pneumonia (lung infection from food entering the lungs)
Getting a PEG is a minor outpatient procedure. Recovery takes days, not weeks. Most people go home the same day. The tube is easy to clean, hidden under clothes, and doesn’t interfere with speech or kissing. It’s not about giving up eating - it’s about keeping your body strong enough to keep breathing.
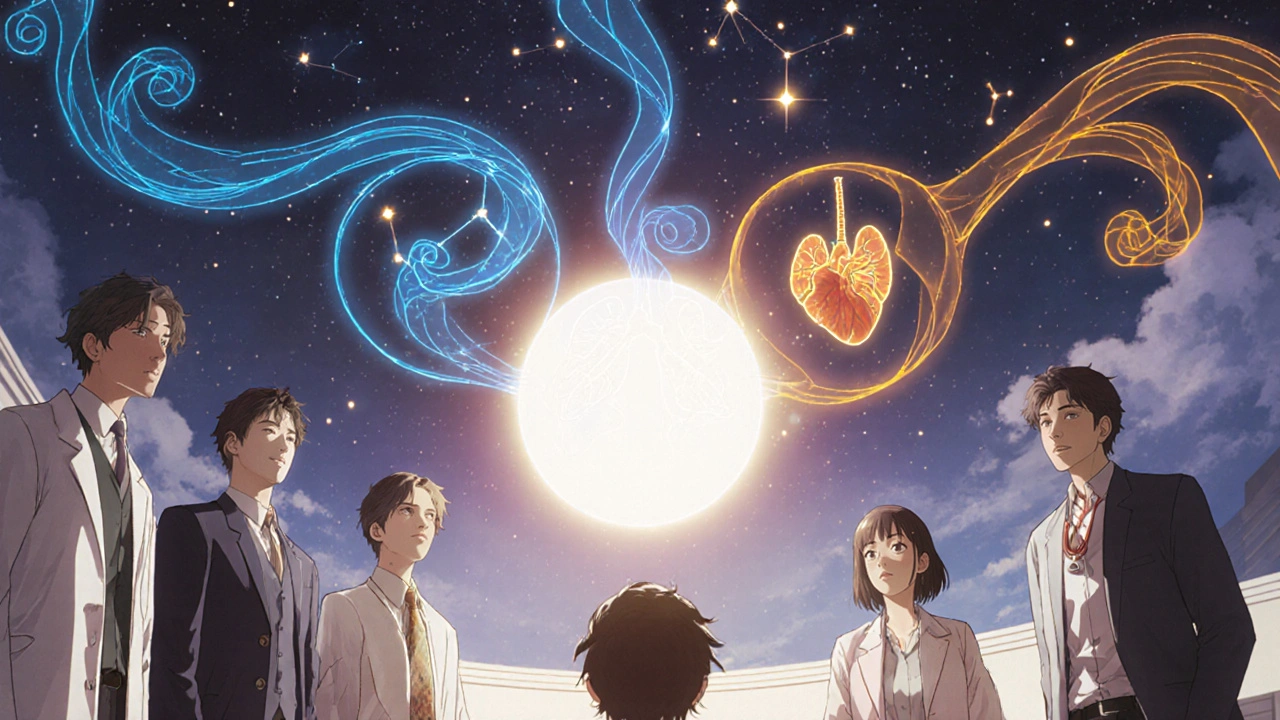
The Big Picture: Together, They Add Over a Year to Life
NIV and PEG aren’t just separate treatments. They work together. A 2021 multinational study found that people who got both interventions lived 12.3 months longer than those who got neither. That’s more than a year. And it’s not magic - it’s science.
One reason? Better nutrition means stronger muscles - including the diaphragm. Better breathing means less fatigue, which means more energy to eat. It’s a cycle. Break one, and the other suffers.
ALS clinics that use a multidisciplinary team - neurologist, respiratory therapist, dietitian, speech pathologist - see a 7.5-month survival advantage over standard care. That’s why the ALS Association now rates clinics on whether they offer NIV counseling and PEG referrals within recommended timeframes. The best centers don’t wait for crises. They plan ahead.
What’s Still Unknown - And What’s Next
Science is still catching up. We don’t yet know which patients will stick with NIV long-term. We don’t have perfect tools to predict who will develop hypercapnia (high CO2) before it’s dangerous. And insurance still holds people back.
But the direction is clear: early action saves lives. You don’t need to be at your worst to get help. You need to be proactive. If you or someone you love has ALS, ask these questions:
- What’s my FVC today? Has it dropped below 80%?
- Am I having trouble sleeping or waking up tired?
- Have I lost more than 5% of my weight in the last 3 months?
- Has anyone talked to me about NIV or a PEG tube?
If the answer to any of those is no - ask again. Push. Get a second opinion. These aren’t decisions to delay. They’re lifelines.
Can I use NIV during the day, or just at night?
Yes, especially as ALS progresses. Standard BiPAP machines are meant for nighttime use. But portable ventilators like the Trilogy 100/106 are designed for daytime use too. They’re lightweight, battery-powered, and can support breathing during meals, walking, or sitting. Many patients start using them during meals to reduce fatigue and improve nutrition.
Does using NIV mean I’ll be on a ventilator forever?
No. NIV is noninvasive - it doesn’t require a tracheostomy. It’s a mask that delivers air pressure. It supports your breathing without replacing it. You can stop using it at any time. Many people use it only at night for years. As the disease advances, some switch to invasive ventilation, but that’s a personal choice, not a requirement.
Is a PEG tube painful or dangerous?
The procedure is done under light sedation and takes less than 30 minutes. Most people go home the same day. The risk of infection is low - under 5% - and easily managed. The tube itself is quiet and hidden. It doesn’t hurt to touch. Many patients say the biggest change is relief: no more choking, no more fear of not eating enough, no more weight loss.
Can I still eat regular food after getting a PEG tube?
Absolutely. The PEG tube doesn’t replace eating - it supplements it. Many people continue to enjoy meals with family, taste their favorite foods, and eat what they can swallow safely. The tube just ensures they get enough calories and protein when swallowing becomes too hard or risky. It’s about quality of life, not giving up.
Why do insurance companies delay approving NIV?
Many insurers still require strict lab values - like FVC below 50% or MIP below -60 cm H2O - even though guidelines say to start earlier based on symptoms. This creates a gap where people suffer unnecessarily. If your doctor recommends NIV but insurance denies it, ask for a letter of medical necessity. Cite the American Academy of Neurology and Canadian Thoracic Society guidelines. Many denials are overturned on appeal.
How do I know if NIV is working?
Look for these signs: fewer morning headaches, better sleep, more energy during the day, less shortness of breath while eating or talking. Your doctor can also check blood gases - if your CO2 drops below 45 mmHg and oxygen stays above 92%, it’s working. Most modern machines also track usage - aim for at least 4 hours per night, ideally more.


King Over
November 20, 2025 AT 07:07Wore it 8 hours a night. Still ate pizza. Still watched football.
Didn’t fix ALS. Made living with it bearable.
Johannah Lavin
November 20, 2025 AT 13:46Ravinder Singh
November 22, 2025 AT 03:07Russ Bergeman
November 23, 2025 AT 07:02Dana Oralkhan
November 25, 2025 AT 03:35Find a good respiratory therapist. Ask for a demo. Try three masks. Don’t let fear make the decision for you. You’ve got this.
Jeremy Samuel
November 26, 2025 AT 13:38Destiny Annamaria
November 27, 2025 AT 04:21Ron and Gill Day
November 28, 2025 AT 22:37Alyssa Torres
November 29, 2025 AT 09:30Summer Joy
November 29, 2025 AT 18:02Shiv Karan Singh
November 30, 2025 AT 12:03Ravi boy
December 1, 2025 AT 02:55Matthew Karrs
December 2, 2025 AT 20:27Matthew Peters
December 3, 2025 AT 20:15