Chronic pain doesn’t just hurt. It wears you down-sleepless nights, canceled plans, the constant fear that the next flare-up will steal another day. And after years of pills, injections, and physical therapy that didn’t deliver real relief, many people feel like they’ve run out of options. That’s where CBT for chronic pain comes in-not as a magic fix, but as a proven way to take back control when the pain won’t go away.
What CBT for Chronic Pain Actually Does
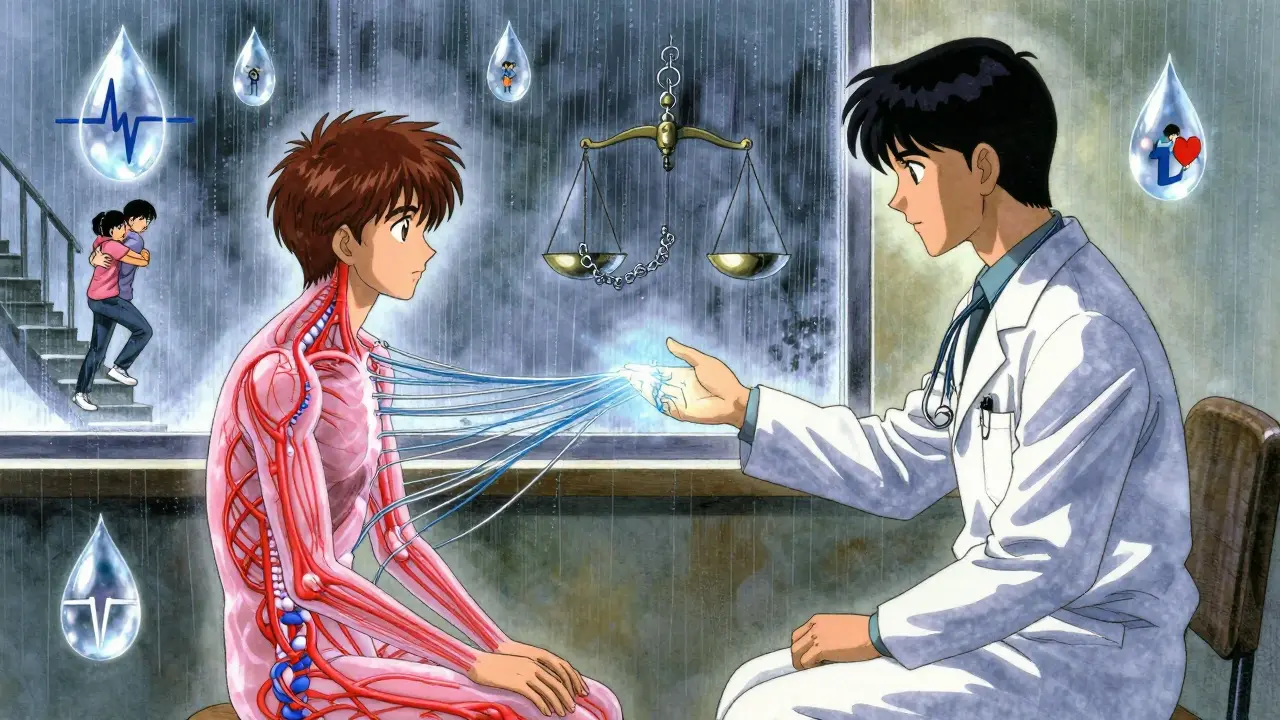
Cognitive Behavioral Therapy for Chronic Pain, or CBT-CP, isn’t about pretending your pain isn’t real. It’s about changing how your brain reacts to it. When pain lasts for months or years, your nervous system gets stuck in overdrive. Your thoughts spiral: “This will never get better,” “I can’t do anything,” “If I move, it’ll get worse.” These thoughts trigger fear, tension, and avoidance. And that cycle makes the pain feel even worse. CBT-CP breaks that cycle. It’s not therapy to “fix your mind.” It’s training for your nervous system. Developed in the 1970s and now used by the U.S. Department of Veterans Affairs and major hospitals, CBT-CP gives you practical tools to manage pain without relying only on meds. You learn to spot when your thoughts are making things harder, how to pace your activity so you don’t crash, and how to calm your body’s stress response.How It Works: The Core Tools
Most CBT-CP programs last between 8 and 16 weeks, with weekly 60- to 90-minute sessions. Whether done in person or online, the structure stays the same. Here’s what you’ll actually do:- Pain neuroscience education: You learn how pain works in the body-not just as damage, but as an output of your brain. This isn’t academic. It helps you stop blaming yourself for pain that doesn’t show up on an X-ray.
- Activity pacing: Instead of doing too much on a good day and crashing for days after, you learn to spread tasks evenly. Think of it like charging a phone: small, consistent use keeps you going longer.
- Cognitive restructuring: You write down thoughts like “I’m broken” or “I’ll never walk normally again,” then challenge them with evidence. Did you walk to the mailbox yesterday? That’s proof you’re not broken.
- Relaxation techniques: Deep breathing, progressive muscle relaxation, and mindfulness help lower your body’s stress response, which directly reduces pain sensitivity.
- Behavioral activation: You rebuild routines you’ve given up-not because the pain is gone, but because living well matters more than waiting to feel perfect.
What the Research Says
A 2023 review of 13 studies with over 1,600 people found CBT-CP consistently improves mood, sleep, and daily function. For depression and anxiety linked to pain, the effect was strong-bigger than most medications. But for pain intensity? The results were mixed. Only about 25% of studies showed a noticeable drop in pain scores. That doesn’t mean it doesn’t work. It means CBT-CP works differently than a painkiller. Think of it like this: If you have a broken leg, you need a cast. But if you’ve had chronic back pain for five years, the problem isn’t just the disc-it’s your brain’s alarm system. CBT-CP turns down the volume on that alarm. You still feel the pain, but it doesn’t control your life. One major 2024 trial (the STAMP study) compared CBT-CP with mindfulness therapy in 254 people on long-term opioids. Both worked equally well at improving function and reducing pain. But here’s the kicker: 36% of people in the CBT group cut their daily opioid use by half or more. Only 17% did in the usual care group. That’s not small. That’s life-changing.Who Benefits Most?
CBT-CP isn’t a one-size-fits-all. It works best for people with:- Chronic low back pain
- Fibromyalgia
- Arthritis
- Pain with anxiety or depression
How It Compares to Other Treatments
| Treatment | Effect on Pain Intensity | Effect on Function | Side Effects | Long-Term Use |
|---|---|---|---|---|
| CBT for Chronic Pain | Moderate to small | Strong improvement | None | Skills last a lifetime |
| Opioid Medications | Moderate (short-term) | Minimal | Dependence, constipation, overdose risk | Not recommended long-term |
| Physical Therapy | Moderate | Strong improvement | Muscle soreness | Requires ongoing sessions |
| Mindfulness Therapy | Moderate | Strong improvement | None | Skills last a lifetime |
| Acupuncture | Small to moderate | Moderate | Rare bruising | Needs repeated sessions |
CBT-CP doesn’t beat physical therapy at improving movement. But it beats it at reducing fear, anxiety, and opioid use. When combined with physical therapy? That’s the gold standard. Patients in one study saw 40% greater improvement in function than with CBT alone.
Real Stories From Real People
On Reddit’s r/ChronicPain, one user wrote: “I used to avoid stairs. Now I take them one at a time. CBT didn’t take my pain away. But it gave me back my life.” Another said: “I cut my oxycodone in half after 10 sessions. I didn’t know I could do that.” A veteran from Texas shared: “I thought therapy was for people who were ‘crazy.’ Turns out, my brain was just stuck. Learning to pace my days saved me from another surgery.” But not everyone wins. Some say: “It felt like they were blaming me for my pain.” Others say: “I couldn’t focus during flare-ups.” That’s why therapist skill matters. A good CBT-CP provider doesn’t dismiss your pain-they help you live with it better.Barriers to Getting Help
The biggest problem? Access. Only 68% of U.S. private insurers cover enough CBT sessions to make a difference. Medicare gives you 10 sessions a year-but you need 12 to 16. Many therapists are in cities, not small towns. And primary care doctors rarely refer patients. But things are shifting. Telehealth CBT is just as effective as in-person, according to a 2021 study. Digital apps like PainCare and CBT-i Coach are now FDA-cleared for chronic pain. And the NIH is investing $14.2 million to make CBT-CP faster, cheaper, and smarter.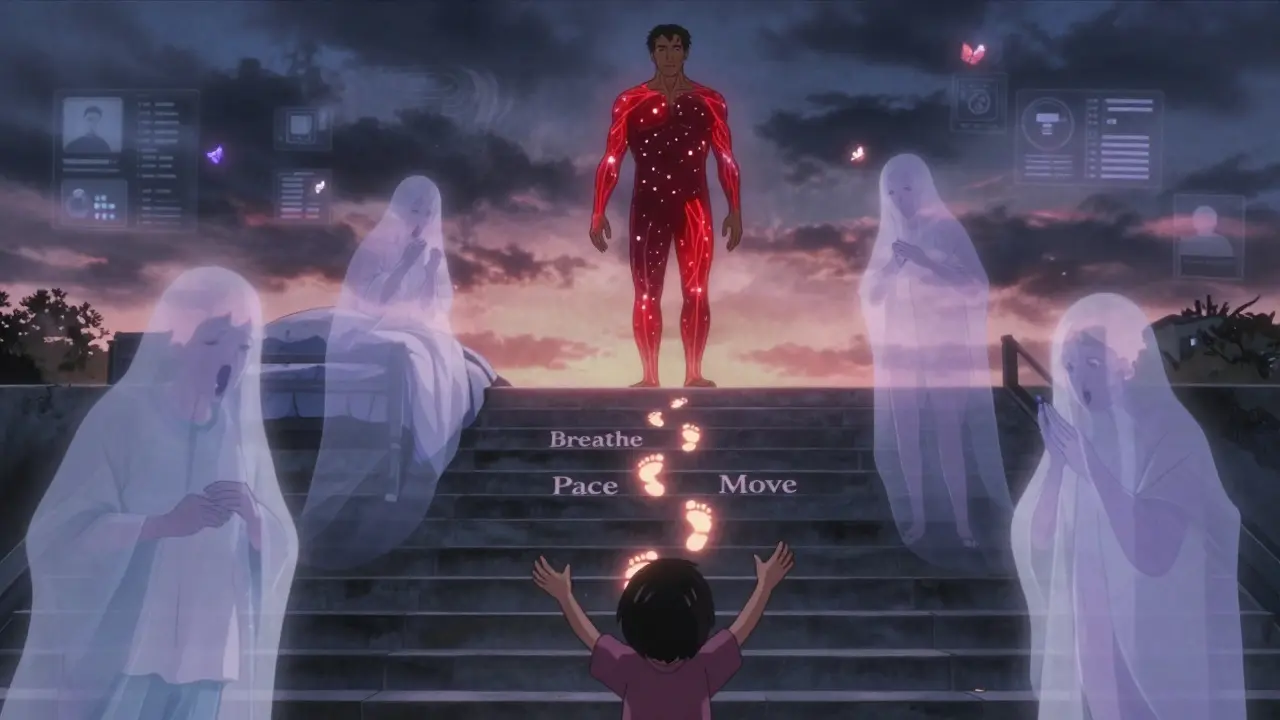
How to Get Started
If you’re ready to try CBT-CP:- Ask your doctor for a referral to a psychologist trained in CBT for chronic pain. Look for “CBT-CP” or “pain psychology” in their specialty.
- Check your insurance. Call and ask: “Do you cover CBT for chronic pain? How many sessions?”
- Consider online programs. The VA offers a free, evidence-based CBT-CP program online. Other platforms like PainCare and MyPainCoach are affordable and accessible.
- Be ready to do the work. CBT-CP isn’t passive. You’ll get homework: journaling, tracking activities, practicing breathing. Skip it, and it won’t work.
- Combine it with movement. Even 10 minutes of walking a day helps CBT-CP stick.
Don’t wait for the pain to disappear before you start living. Start now. You don’t need to be pain-free to be present.
What to Expect in the First Few Weeks
The first session feels like a conversation. You’ll talk about your pain history, what you’ve tried, and what you want to change. The therapist won’t give you a magic answer. Instead, they’ll ask: “What’s one thing you’d like to do this week that you’ve avoided because of pain?” Week 2: You’ll start tracking your pain and activity. You might log: “Walked to mailbox-pain 6/10. Felt guilty afterward.” That’s normal. That’s data. Week 4: You’ll begin challenging thoughts. “I can’t do anything” becomes “I did X, and it was hard, but I did it.” Week 8: You’ll start planning for setbacks. “If I have a bad day, I’ll use my breathing technique and rest, then do one small thing tomorrow.” It’s not fast. But it’s lasting.Is CBT for chronic pain just in my head?
No. CBT doesn’t mean your pain isn’t real. It means your brain has learned to respond to pain in ways that make it worse. CBT helps retrain that response. Think of it like physical therapy for your nervous system. Just as a torn muscle needs rehab, a sensitized pain system needs rewiring. The pain is physical-but how you react to it can be changed.
How long until I see results from CBT for chronic pain?
Most people notice changes in mood, sleep, or activity levels within 4 to 6 weeks. Pain intensity may not drop right away. The real wins come in how you live: fewer canceled plans, less fear of movement, reduced reliance on pills. By week 10, people report feeling more in control-even if the pain is still there.
Can I do CBT for chronic pain on my own?
You can start with apps or workbooks, but working with a trained therapist gives you better results. A therapist helps you spot blind spots-like when you’re avoiding activity because of fear, not pain. They also adjust your plan if something isn’t working. Self-guided CBT helps, but guided CBT is 2 to 3 times more effective, according to clinical studies.
Does CBT for chronic pain work for everyone?
Not everyone. It works best for people who are motivated to change how they respond to pain-not to eliminate it. Those with severe depression, cognitive impairments, or who are not ready to take responsibility for their recovery may struggle. Also, it’s less effective for pure nerve pain. But for most with musculoskeletal pain and emotional distress, it’s one of the most powerful tools available.
What if I can’t afford CBT for chronic pain?
The VA offers free CBT-CP online to veterans. Many universities with psychology programs offer low-cost clinics staffed by supervised trainees. Apps like PainCare and CBT-i Coach cost under $20/month. Some nonprofits provide scholarships. And telehealth has made it easier to find affordable options-even if you live in a rural area.


Dan Gaytan
December 23, 2025 AT 11:11This is the kind of post that makes me want to hug the internet. CBT for chronic pain isn't about denying your suffering-it's about reclaiming your life from it. I've been through it, and the pacing technique alone saved me from burning out every other week. You don't need to be fixed. You just need to learn how to move with the pain, not against it.
Also, that opioid reduction stat? 36%? That’s not just data-that’s people getting their lives back. Thank you for sharing this.
Steven Mayer
December 24, 2025 AT 02:48The neuroplasticity component is understated here. CBT-CP modulates descending inhibitory pathways via prefrontal-limbic recalibration, reducing central sensitization through top-down regulation of nociceptive processing. The behavioral activation component isn’t just ‘doing things’-it’s counterconditioning avoidance behaviors that reinforce pain catastrophizing. The literature supports this as a neuromodulatory intervention, not merely psychological coping.
Bret Freeman
December 26, 2025 AT 02:21Look, I get it. People want a magic bullet. But this isn’t therapy-it’s a corporate wellness scam wrapped in science-speak. They’re just trying to get you to stop complaining so insurance doesn’t have to pay for real treatment. I’ve been in pain for 12 years. They don’t care if you walk again. They just want you to shut up and take a breathing app.
And don’t even get me started on ‘pacing.’ That’s just another way to say ‘live smaller.’
Lindsey Kidd
December 27, 2025 AT 22:58❤️ This. So much this. I was skeptical too-until I started journaling my pain triggers and realized I was avoiding my own life. I didn’t know I could still dance in the kitchen with my kid, even with a 7/10 pain day. CBT didn’t fix me. It reminded me I was still here.
And to anyone saying ‘it’s all in your head’-no. It’s in your nervous system. And yours can learn.
Austin LeBlanc
December 28, 2025 AT 08:33Wait-you’re telling me I should stop taking opioids and do breathing exercises instead? That’s what the doctors want? That’s why my sister died of an overdose last year? You think her pain wasn’t real? You think CBT would’ve saved her? Don’t you dare gaslight people who are in real, unbearable pain with this feel-good nonsense.
I’ve seen too many people told to ‘just think positive’ while their spine collapses. This isn’t empowerment. It’s abandonment dressed up as therapy.
Gray Dedoiko
December 30, 2025 AT 02:30I’ve done CBT-CP. It’s not easy. Some weeks I skipped homework. Some days I cried because I felt like I was failing. But I kept going because my therapist didn’t judge me for it. The thing nobody talks about? It’s not about pain going away. It’s about the guilt fading. The shame. The fear that you’re lazy because you can’t do what you used to.
That’s what changed for me.
Paula Villete
December 30, 2025 AT 15:31Of course CBT works-because it’s the only thing insurance will cover. Meanwhile, the real issue-chronic inflammation, undiagnosed autoimmune flares, nerve compression-is ignored because ‘it’s psychological.’
Let’s call it what it is: a cost-saving band-aid for a system that refuses to treat chronic pain as a medical emergency. Brilliant strategy. Shame it’s not actually medicine.
Georgia Brach
December 30, 2025 AT 17:08The data is cherry-picked. You cite a 2023 review, but omit that 60% of CBT-CP studies show no clinically significant change in pain intensity. You highlight opioid reduction without mentioning the 40% who dropped out due to frustration. You present this as a cure-all while ignoring the populations it fails-elderly, neurodivergent, low-literacy, non-English speakers.
This isn’t science. It’s marketing.
Katie Taylor
December 31, 2025 AT 01:46STOP TELLING PEOPLE TO JUST ‘ACCEPT’ THEIR PAIN. That’s not therapy-that’s giving up. You think someone with fibromyalgia wants to ‘pace’? They want their body to stop betraying them. CBT is a Band-Aid on a hemorrhage. If you’re not pushing for better meds, better diagnostics, better research-you’re part of the problem.
I’ve done CBT. It helped my anxiety. It didn’t help my pain. Don’t confuse the two.
Payson Mattes
December 31, 2025 AT 07:27Did you know the NIH is funding CBT because Big Pharma doesn’t want you to know that chronic pain is caused by 5G radiation and microchips implanted during vaccines? They’re pushing CBT to make you think it’s all in your head so they can keep selling useless pills while the real cause stays hidden. I know someone who got cured after removing their dental fillings. You’re being manipulated.
Also, the VA program? They track your thoughts. Don’t let them know you’re mad.
Bhargav Patel
January 1, 2026 AT 02:25While the empirical efficacy of CBT-CP is well-documented in randomized controlled trials, one must critically examine the epistemological assumptions underlying its framework. The model presumes a Cartesian separation between mind and body, wherein cognitive restructuring is posited as a corrective mechanism for somatic pathology. This ontological dualism, however, is increasingly contested in contemporary pain neuroscience, which emphasizes embodied cognition and neurophenomenological integration. Thus, while CBT-CP may yield functional improvements, its theoretical foundation remains reductionist.
Charles Barry
January 2, 2026 AT 03:11Of course it works. Because the system wants you to believe you can fix yourself. That way, they don’t have to fund real treatment. You think they care about your pain? They care about your insurance premiums. CBT is cheaper than MRI scans. It’s cheaper than surgery. It’s cheaper than listening. And now they’ve turned it into a cult. ‘Just breathe, just reframe, just be grateful.’
Meanwhile, your spine is crumbling. Your nerves are screaming. And they’re handing you a journal.