Doctors don’t know how much your pills cost - and it’s costing you money
Imagine your doctor writes you a prescription for a common medication. You pick it up at the pharmacy, swipe your card, and see a $200 bill. You’re stunned. You thought this was a cheap, generic drug. Your doctor did too. But they were wrong - by more than 150%.
This isn’t a rare mistake. It’s standard.
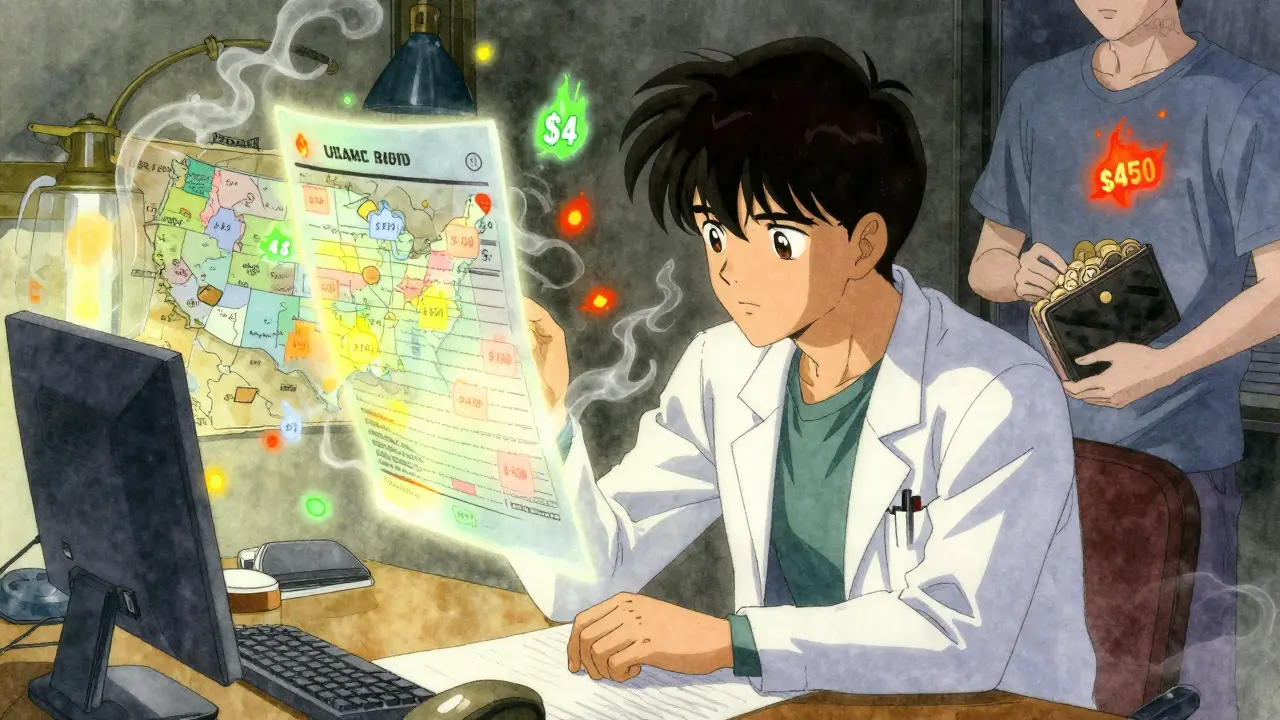
Studies show that most clinicians grossly misjudge drug prices. They overestimate the cost of cheap generics by nearly a third and underestimate expensive brand-name drugs by over 70%. That means doctors are often prescribing high-cost drugs thinking they’re being frugal - and patients are left footing the bill.
The U.S. spends over $600 billion a year on prescription drugs. Eighty-two percent of adults say those prices are unreasonable. Yet most doctors have no idea what those prices actually are.
How bad is the knowledge gap?
A 2016 study of 254 medical students and doctors found that only 5.4% of generic drug costs were estimated within 25% of the actual price. For brand-name drugs, it was just 13.7%. That’s worse than random guessing.
Doctors thought a $4 generic blood pressure pill cost $12. They thought a $450 diabetes drug cost $120. In one case, a $15 insulin vial was estimated at $300. These aren’t outliers - they’re the norm.
Even more troubling: 77.5% of the time, doctors overestimated the cost of generic drugs. Why? Because they assume generics are expensive. They’re not. Most cost less than $10. But without real-time data, they default to guesswork.
Medical students are even worse. Only 40% could name even one source for drug pricing info. By the time they become residents, that number climbs - but barely. Median knowledge scores on drug pricing questions hover around 6 out of 10.
Why don’t doctors know?
It’s not laziness. It’s not ignorance. It’s structure.
Drug prices aren’t fixed. A pill can cost $15 at one pharmacy, $320 at another. It depends on your insurance, your deductible, your pharmacy network, and whether you’ve hit your out-of-pocket maximum. There’s no single price tag.
Most EHR systems don’t show real-time costs. When they do, they often show wholesale prices - not what you pay. One resident on Reddit complained: “Our Epic system shows insurer pricing, but not my patient’s copay. It’s useless.”
Doctors don’t have time to look it up. Checking costs takes 3 to 5 minutes per prescription. In a packed clinic, that’s 30 extra minutes a day. That’s a whole patient slot gone.
And most medical schools don’t teach it. Fifty-six percent of U.S. med schools have no formal curriculum on drug pricing. Students graduate thinking drug costs reflect R&D expenses - when in reality, only 16% of price hikes are tied to innovation. The rest? Marketing, profit, and patent extensions.
What’s changing - and what’s not
Some hospitals are fixing this. UCHealth in Colorado rolled out real-time benefit tools (RTBTs) in their EHR in 2022. When a doctor selects a drug, a pop-up shows the patient’s estimated out-of-pocket cost - based on their actual insurance plan.
Result? One in eight doctors changed their prescription. When potential savings hit $20 or more, that number jumped to one in six.
Patients saved an average of $187 per year. That’s not a rounding error. That’s a month’s rent for some.
But only 37% of U.S. hospitals have these tools. Most still rely on outdated formularies, printed guides, or Google searches. Mayo Clinic’s Drug Cost Resource Guide gets a 4.7/5 rating from its users. Medicare’s Part D formulary? Just 2.8/5.
Even when tools exist, they’re clunky. They don’t always update. They don’t account for coupons, cash discounts, or pharmacy loyalty programs. And they often don’t work for patients on Medicaid or Medicare Advantage plans.
Who’s paying the price?
Patients. Always patients.
Twenty-eight percent of Americans skip doses or don’t fill prescriptions because of cost. That’s 70 million people. And doctors - unaware of the true price - keep prescribing expensive options.
It’s worse for low-income patients. Preliminary data from safety-net clinics shows RTBTs lead to 22% higher prescription changes in these settings than in private practices. Why? Because when you’re choosing between insulin and rent, $150 matters.
And it’s not just about generics. A 2024 report found drug prices for Humira, Januvia, and other top sellers rose by 4.7% to 8.3% - with no new clinical benefit. Doctors prescribing these drugs weren’t told. Patients weren’t told. The system just kept billing.
Can we fix this?
Yes - but not by hoping doctors memorize prices.
Real change needs three things:
- Integrated cost data in EHRs - not just wholesale prices, but patient-specific out-of-pocket estimates pulled from insurers in real time.
- Training in medical school - every med student should learn how drug pricing works, how to find alternatives, and how to talk to patients about cost.
- Accountability - if a hospital claims to provide high-value care, it should track how often expensive drugs are prescribed when cheaper, equally effective options exist.
Doctors under 40 are already adopting these tools faster - 78% vs. 52% for those over 55. That’s a generational shift. Younger clinicians grew up with smartphones, apps, and instant data. They don’t want to guess. They want to know.
The Inflation Reduction Act gave Medicare power to negotiate drug prices. That’s a start. But it won’t help patients on private insurance - and it won’t fix the knowledge gap.
What will fix it? Making cost visibility as routine as checking a patient’s blood pressure.
What patients can do
You don’t have to wait for your doctor to catch up.
Before your appointment, use free tools like GoodRx, SingleCare, or your insurer’s price checker. Know what your cheapest option is - even if it’s a different brand or dosage.
Ask your doctor: “Is there a cheaper alternative?” or “What does this cost out-of-pocket?” Don’t be shy. It’s your money. And your health.
Most doctors will appreciate the question. They want to help - they just didn’t have the tools.
The future is visible
By 2027, 75% of U.S. health systems are expected to have advanced cost-alert tools. That’s a massive shift - from guesswork to transparency.
But technology alone won’t fix this. We need to stop treating drug pricing as a secret. It’s not a business secret. It’s a public health issue.
When doctors know the real cost, they prescribe better. Patients take their meds. Health improves. Costs drop.
The data is clear. The tools exist. The will is growing.
Now it’s just a matter of making sure every doctor - and every patient - can see the price before they say yes.
Why don’t doctors know how much drugs cost?
Doctors don’t know because drug prices aren’t standardized - they vary by insurance, pharmacy, and patient-specific factors like deductibles. Most electronic health record systems don’t show real-time, patient-specific costs, and medical schools rarely teach pricing. Even when tools exist, they’re often outdated or inaccurate, making it easier to guess than to check.
Are generic drugs really cheaper than brand-name drugs?
Yes - and most doctors underestimate just how much. Generic drugs are chemically identical to brand-name versions but cost 80-85% less on average. A common blood pressure generic like lisinopril costs about $4 for a 30-day supply. Many doctors think it’s $10-$15. This misunderstanding leads to unnecessary prescriptions of more expensive alternatives.
Do cost alerts in EHR systems actually change prescriptions?
Yes. Studies show that when doctors see real-time out-of-pocket costs during prescribing, one in eight change their prescription - rising to one in six when potential savings exceed $20. UCHealth’s system, for example, led to a 12.5% reduction in high-cost prescriptions after introducing cost alerts.
Can patients help doctors make better prescribing decisions?
Absolutely. Patients can use free tools like GoodRx or their insurer’s price checker to find the lowest-cost option before their appointment. Asking, “Is there a cheaper alternative?” or “What’s this going to cost me?” gives doctors the context they need - and often leads to better, more affordable care.
Why do drug prices vary so much between pharmacies?
Drug prices vary because pharmacies negotiate separate contracts with insurers and pharmacy benefit managers (PBMs). A drug might cost $15 at Walmart with a cash discount but $320 at a specialty pharmacy if your insurance doesn’t cover it. There’s no national price - just a tangled web of private deals that patients and doctors rarely see.
Is the Inflation Reduction Act helping with drug pricing transparency?
It’s a step forward, but not a full solution. The law lets Medicare negotiate prices for 10 high-cost drugs starting in 2026 - lowering costs for seniors. But it doesn’t directly affect private insurance patients or make prices visible at the point of care. True transparency requires EHR integration, not just government negotiation.

Ellie Stretshberry
December 27, 2025 AT 03:21Dan Alatepe
December 28, 2025 AT 11:46Joanne Smith
December 29, 2025 AT 02:42Sarah Holmes
December 29, 2025 AT 14:07jesse chen
December 29, 2025 AT 15:33Zina Constantin
December 31, 2025 AT 10:22christian ebongue
January 2, 2026 AT 04:19Prasanthi Kontemukkala
January 3, 2026 AT 02:30Angela Spagnolo
January 4, 2026 AT 23:48Shreyash Gupta
January 6, 2026 AT 18:54Jody Kennedy
January 8, 2026 AT 08:25