If you’ve had heartburn for years-maybe even decades-you might think it’s just part of life. But chronic GERD isn’t just uncomfortable. It’s a silent driver behind one of the most dangerous cancers you’ve never heard of: esophageal cancer. The good news? Most people never develop it. The bad news? If you’re in a high-risk group and ignore the warning signs, you could be walking into a late-stage diagnosis with a 21% chance of surviving five years.
How GERD Turns Into Cancer
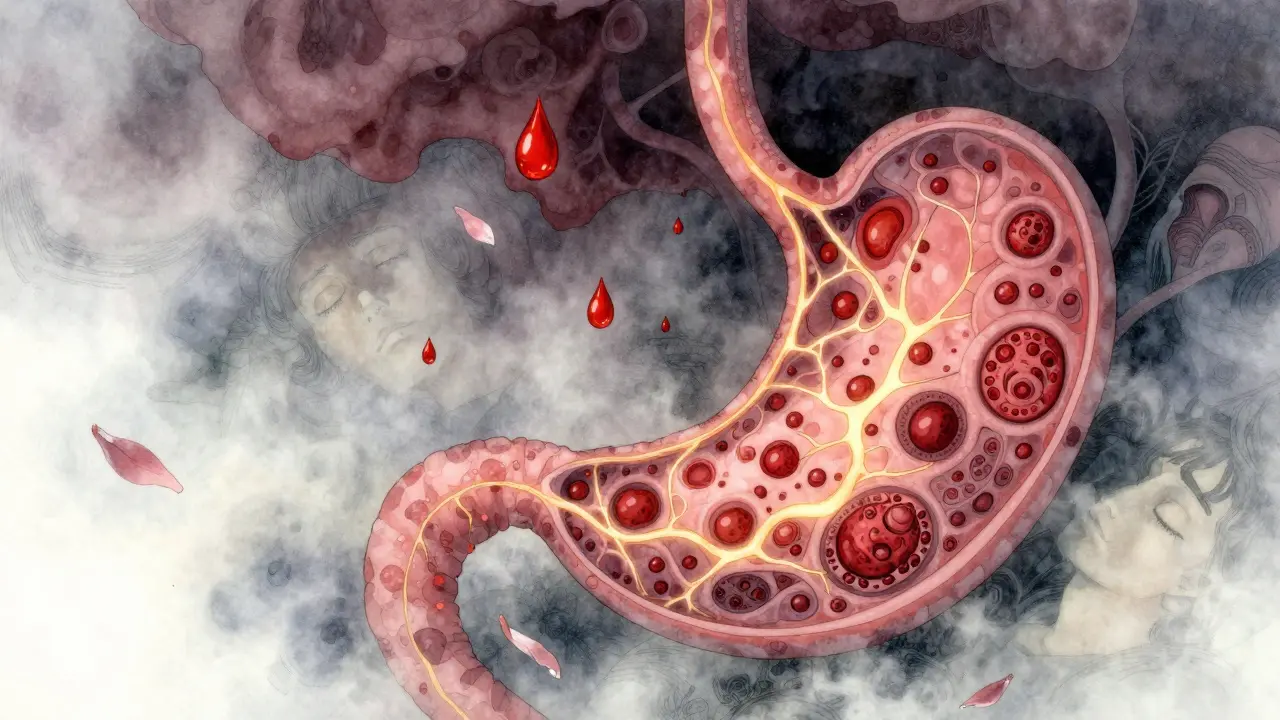
Your esophagus isn’t designed to handle stomach acid. Every time acid backs up, it burns the delicate lining. Over time, your body tries to protect itself by changing the cells in the esophagus to look more like stomach cells. That’s called Barrett’s esophagus. It’s not cancer. But it’s the only known precursor to esophageal adenocarcinoma, the most common type of esophageal cancer in the U.S. According to a 2023 NIH study, people with chronic GERD have a 3.2 times higher risk of developing esophageal cancer than those without it. That’s not a small increase. It’s the strongest known risk factor. And the longer you have GERD, the worse it gets. Five years of symptoms? That’s the tipping point. Ten years? Your risk jumps even higher. And if you’re having symptoms weekly, your risk is seven times greater than someone with no reflux. This isn’t a fast process. It takes years. That’s why so many people don’t connect their heartburn to cancer. But here’s the catch: once Barrett’s esophagus develops, the chance of it turning into cancer is low-only 0.2% to 0.5% per year. Still, with millions of Americans suffering from GERD, that small percentage adds up fast. That’s why early detection matters more than ever.Who’s Actually at Risk?
Not everyone with GERD gets Barrett’s esophagus. Only about 10-15% of chronic GERD patients do. But certain people are far more likely to cross that line. The biggest risk factors aren’t guesses-they’re backed by data:- Male: Men are 3 to 4 times more likely than women to develop esophageal adenocarcinoma.
- Over 50: 90% of cases happen in people over 55. If you’re 50+ and have GERD, you’re in the danger zone.
- White, non-Hispanic: White Americans have three times the rate of adenocarcinoma compared to Black Americans.
- Obese (BMI 30+): Extra weight squeezes your stomach, forcing acid upward. Obesity causes 30-40% of GERD cases.
- Smoker: Smoking doubles or triples your risk. And if you smoke AND have GERD? The risk multiplies.
- Family history: If a close relative had esophageal cancer, your risk goes up.
The Red Flags No One Talks About
Most people with early-stage esophageal cancer feel fine. That’s why it’s called a silent killer. But when symptoms do show up, they’re not subtle. Here’s what you need to watch for:- Dysphagia: Trouble swallowing. It starts with solids-chicken, bread, meat-and slowly moves to liquids. This is the most common symptom, present in 80% of cases at diagnosis.
- Unexplained weight loss: Losing 10 pounds or more in six months without trying? That’s a major red flag.
- Food getting stuck: That feeling that something’s lodged in your chest or throat? It’s not just indigestion. It happens in 30-40% of cases.
- Chronic hoarseness or cough: If your voice is raspy or you’re coughing constantly for more than two weeks, it could be acid irritating your throat and vocal cords.
- Heartburn that won’t quit: If you’ve had heartburn more than twice a week for five or more years, you’re not just “sensitive to spicy food.” You’re in the high-risk group.

What You Can Do to Lower Your Risk
The good news? You have control over most of this. You can’t change your age or gender, but you can change your habits-and the data shows it works.- Quit smoking: Within 10 years of quitting, your cancer risk drops by half.
- Lose weight: Shedding just 5-10% of your body weight reduces GERD symptoms by 40%. That’s not just about comfort-it’s about preventing cancer.
- Limit alcohol: One drink a day for women, two for men. Heavy drinking doesn’t raise adenocarcinoma risk much, but it spikes another type of esophageal cancer. Better safe than sorry.
- Take PPIs consistently: If you’ve been diagnosed with Barrett’s esophagus, taking proton pump inhibitors (like omeprazole or esomeprazole) every day for five years cuts your cancer risk by 70%.
- Get screened: If you’re in the high-risk group, an endoscopy is the only way to see if you have Barrett’s esophagus. It’s quick, safe, and done under mild sedation. The biopsy can catch precancerous changes before they turn deadly.
What’s Changing in Screening
Endoscopy is still the gold standard, but it’s invasive. That’s why new tools are emerging. One promising option is the Cytosponge-a pill-sized sponge on a string you swallow. It collects cells from your esophagus as it’s pulled back out. In a 2022 Lancet study, it detected Barrett’s esophagus with 79.9% accuracy. No scopes. No sedation. Just a quick, painless test. Doctors are also using tools like narrow-band imaging and laser microscopes during endoscopy to spot abnormal tissue better. And there’s a new risk calculator called BE MAPPED that uses seven factors-age, sex, BMI, smoking, GERD duration, family history, and race-to predict your personal risk with 85% accuracy. It’s not perfect, but it’s a big step toward personalized prevention.
Why This Matters More Than Ever
Since 1975, esophageal adenocarcinoma rates have gone up by 850%. Why? Because obesity and GERD have exploded. In the 1970s, about 15% of Americans were obese. Today, it’s 42%. More weight means more acid reflux. More reflux means more Barrett’s. More Barrett’s means more cancer. The American Cancer Society estimates 21,630 new cases of esophageal cancer in the U.S. in 2023-and 16,780 deaths. That’s because 75% of cases are found too late. But if caught early, when it’s still confined to the esophagus, the five-year survival rate jumps from 21% to 50-60%. This isn’t about scaring you. It’s about giving you power. You can’t ignore GERD forever. But you also don’t need to live in fear. If you’re in a high-risk group, get checked. If you’re not, take steps now to lower your risk. The next time you feel that burn in your chest, don’t just reach for an antacid. Ask yourself: Is this just heartburn… or is it my body trying to tell me something bigger?Can GERD cause cancer even if I take medication?
Yes, but significantly less. Medications like PPIs reduce acid exposure, which lowers the chance of Barrett’s esophagus developing. Studies show consistent PPI use for five or more years cuts cancer risk by 70% in people who already have Barrett’s. But medication doesn’t reverse existing cell changes. That’s why regular monitoring is still needed if you’ve had GERD for over five years.
If I have heartburn every day, does that mean I have Barrett’s esophagus?
Not necessarily. Daily heartburn means you have chronic GERD, which increases your risk of Barrett’s-but only about 10-15% of people with long-term GERD develop it. The only way to know for sure is through an endoscopy and biopsy. Don’t assume you have it. But don’t assume you don’t either.
Is esophageal cancer hereditary?
It can be. Having a first-degree relative (parent, sibling, child) with esophageal cancer increases your risk. But genetics alone rarely cause it. It’s usually a mix of inherited factors and lifestyle-like GERD, smoking, or obesity. If you have a family history, talk to your doctor about earlier screening.
Can I get screened for esophageal cancer without an endoscopy?
There’s a new option called the Cytosponge-a pill you swallow that collects cells from your esophagus. It’s less invasive than an endoscopy and detects Barrett’s esophagus with nearly 80% accuracy. It’s not yet widely available, but it’s being rolled out in some clinics and may become standard in the next few years. For now, endoscopy remains the most reliable method.
Does acid reflux always lead to cancer?
No. In fact, over 85% of people with chronic GERD never develop Barrett’s esophagus, and over 99% never develop cancer. But because GERD affects 20% of the U.S. population, even a small percentage turning into cancer adds up to thousands of cases each year. That’s why it’s important to know your risk and act early if you’re in a high-risk group.

asa MNG
January 23, 2026 AT 15:49Juan Reibelo
January 24, 2026 AT 16:16Sawyer Vitela
January 24, 2026 AT 21:20Kevin Waters
January 25, 2026 AT 03:28Jamie Hooper
January 25, 2026 AT 18:28Himanshu Singh
January 27, 2026 AT 13:56Sushrita Chakraborty
January 28, 2026 AT 16:51Husain Atther
January 30, 2026 AT 09:15Helen Leite
January 30, 2026 AT 16:54Marlon Mentolaroc
February 1, 2026 AT 06:49Darren Links
February 2, 2026 AT 19:26