When you swallow a pill, you expect it to work-but not too fast, not too slow. The difference between extended-release and immediate-release medications isn’t just about how long they last. It’s about safety, effectiveness, and avoiding dangerous mistakes. One wrong move-like crushing a pill or taking an extra dose because you don’t feel it right away-can land you in the ER. And it’s not rare. Thousands of people do this every year, often because they don’t know what’s inside that tablet.
How These Two Types Work
Immediate-release (IR) pills are the classic kind. You take them, and within 15 to 30 minutes, the drug starts dissolving in your stomach. Peak levels hit your bloodstream in under two hours. That’s why IR painkillers like oxycodone or acetaminophen work fast-they’re meant to. But the effect fades quickly, usually within 4 to 8 hours. That’s why people on IR meds often need to take them three or four times a day. Extended-release (ER, XR, SR, CR) pills are engineered differently. They don’t dump everything at once. Instead, they use special coatings, tiny pellets, or slow-dissolving gels to release the drug over 12 to 24 hours. Think of it like a water drip system instead of a firehose. Drugs like metformin XR, Adderall XR, or venlafaxine ER are designed to keep levels steady. No spikes. No crashes. Just steady relief.Why ER Feels Slower-And Why That’s a Good Thing
If you’ve ever taken an ER antidepressant and thought, “This isn’t working,” you’re not alone. Many patients stop after a few days because they don’t feel an instant change. But ER meds take longer to build up. It can take 7 to 10 days to reach full steady-state levels, compared to 3 to 5 days for IR. That’s not a flaw-it’s how they’re supposed to work. Take bupropion. The immediate-release version hits peak levels at 400-600 ng/mL within two hours. That’s enough to trigger seizures in some people if taken in high doses. The extended-release version? It holds steady between 100-200 ng/mL all day. That’s why 300 mg of bupropion XL is safe-but 300 mg of IR could be deadly. The ER version avoids the dangerous peaks that cause side effects.When IR Is the Better Choice
ER isn’t always better. Sometimes, you need speed. For acute pain, breakthrough anxiety, or sudden panic attacks, IR wins. An ER opioid might take 2 to 4 hours to kick in. If you’re in severe pain, that’s too long. That’s why doctors often prescribe IR versions for rescue doses-even if the main treatment is ER. Same goes for ADHD. Adderall XR gives you 10-12 hours of focus. But if you have a big presentation and need a quick boost, keeping a 5 mg IR tablet on hand makes sense. Many patients use both: ER for daily stability, IR for those moments when you need an instant lift.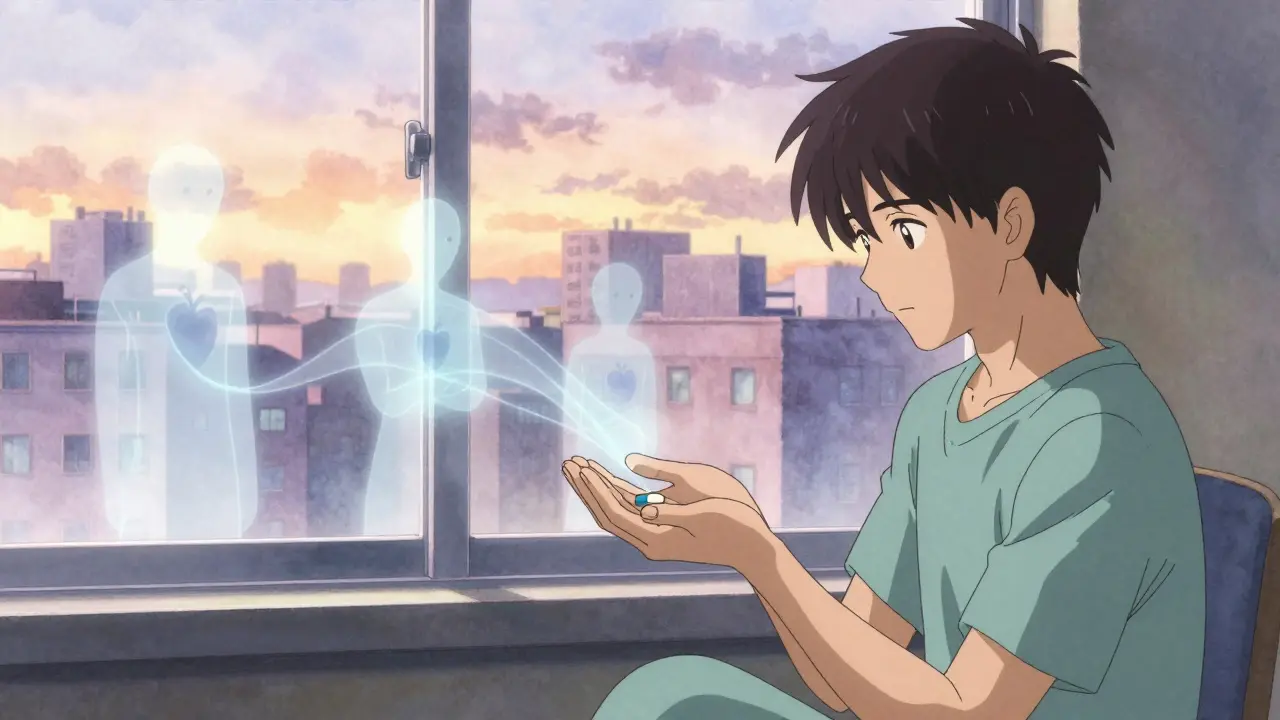
The Hidden Risks of ER Medications
Here’s where things get dangerous. Almost all ER pills are designed to be swallowed whole. Crush them. Chew them. Split them. And you’re basically giving yourself a full dose all at once. The FDA issued a warning in 2020 about extended-release opioids. People who crushed them to snort or inject ended up with fatal overdoses because the entire dose released immediately. The same applies to ER stimulants, antidepressants, and even blood pressure meds like metoprolol ER. One patient split a 100 mg metoprolol XR tablet, thinking it would help her anxiety faster. She ended up with dangerously low blood pressure and a hospital stay. And here’s the kicker: 92% of ER formulations can’t be safely altered. Even if a pill looks like it has a score line, that doesn’t mean it’s safe to split. Venlafaxine XR, for example, has a special coating that breaks if you split it. Pharmacists report 23% of medication errors with ER drugs come from people splitting or crushing them.Adherence: Why ER Wins (Most of the Time)
One of the biggest reasons doctors push ER is adherence. If you have to take a pill three times a day, you’re going to miss some. But once or twice? Much easier to remember. A 2022 study in JAMA Internal Medicine tracked 15,000 people on blood pressure meds. Those on ER versions had a 78% adherence rate over 12 months. Those on IR? Only 56%. That’s a 22% gap. Better adherence means fewer hospital visits, fewer complications, and lower long-term costs. Patients on ER antidepressants also report fewer side effects like insomnia or jitteriness. Quetiapine XR, for example, causes less sleep disruption than IR because the drug doesn’t spike at night.Cost and Accessibility
ER versions usually cost 15-25% more than IR. Adderall XR can run $350-$450 for 30 capsules. Adderall IR? Around $280-$380. That’s a real barrier for people without good insurance. But here’s the twist: the higher upfront cost can save money long-term. Fewer missed doses mean fewer ER visits, fewer doctor trips, fewer lab tests. A 2023 study found that patients on ER meds for chronic conditions had 18% lower overall healthcare costs over a year.
Who Should Avoid ER?
ER isn’t for everyone. If you have gastroparesis-a condition where your stomach empties slowly-ER meds can be unpredictable. Your body might hold onto the pill too long, then release it all at once. The FDA warned in July 2023 that patients with gastroparesis can have 30-50% higher peak drug levels, increasing overdose risk. People with severe kidney or liver disease also need caution. ER drugs are designed to be cleared slowly. If your body can’t process them, they build up. That’s why doctors often start these patients on IR first, then switch only if they tolerate it well.What to Do If You’re Unsure
If you’re prescribed an ER medication, ask these three questions:- Is this pill meant to be swallowed whole? (If it’s coated, scored, or labeled XR/ER, the answer is yes.)
- How long should I wait before I feel results? (It’s not 30 minutes-it’s days.)
- What should I do if I miss a dose? (Never double up. Just take the next one on time.)
The Bottom Line
Extended-release and immediate-release aren’t just different forms of the same drug. They’re different tools for different jobs. ER gives you steady, long-lasting control. IR gives you fast, flexible relief. Mixing them up-whether by accident or misunderstanding-can be risky. But when used right, ER reduces side effects, improves adherence, and saves lives. The key is knowing which one you have, how it works, and never, ever tampering with it.Can I split my extended-release pill if it has a score line?
No-not unless the packaging or your doctor specifically says it’s safe. Many scored ER pills still have special coatings or matrices that break when split, causing the full dose to release at once. Even if it looks like it’s designed to be split, assume it’s not unless confirmed by your pharmacist or the manufacturer’s labeling.
Why does my ER medication take so long to work?
Extended-release drugs are built to release slowly, so it takes 7-10 days to reach steady levels in your bloodstream. You won’t feel a big change right away, and that’s normal. If you take extra doses because you don’t feel it, you risk overdose. Give it time. If after two weeks you still feel no benefit, talk to your doctor.
Is it safe to take ER and IR versions of the same drug together?
Sometimes, yes-but only under strict medical supervision. For example, someone on Adderall XR might be given a small IR dose for breakthrough symptoms. But never combine them without your doctor’s direction. Adding IR to ER can push your total dose beyond safe limits, especially with stimulants or opioids.
What happens if I accidentally crush an extended-release pill?
You’ve likely released the entire dose all at once. This can cause a sudden spike in drug levels, leading to overdose symptoms like rapid heartbeat, confusion, seizures, or extreme drowsiness. If this happens, call poison control immediately (1-800-222-1222 in the U.S.) and go to the ER. Do not wait for symptoms to appear.
Are extended-release medications more expensive? Is it worth it?
Yes, ER versions usually cost more upfront-15-25% higher. But they often lead to fewer missed doses, fewer side effects, and less need for emergency care. Over time, this can lower your total healthcare costs. For chronic conditions like high blood pressure, depression, or ADHD, the improved adherence and stability make ER worth the extra cost for most people.
Can I switch from IR to ER without tapering?
Sometimes, but not always. For some drugs like metoprolol or sertraline, switching directly from IR to ER at an equivalent dose is safe. For others, like bupropion or venlafaxine, your doctor may need to adjust the dose or taper slowly to avoid withdrawal or side effects. Never switch on your own. Always consult your prescriber.


Brian Furnell
December 21, 2025 AT 03:49Okay, so let me get this straight: ER meds are like a slow-burn candle, and IR is a firecracker? I’ve been taking metformin XR for three years and thought the ‘delayed effect’ was just my imagination. Turns out, my pancreas is just chillin’ while my blood sugar gets a steady massage. Also-92% of ER pills shouldn’t be crushed? That’s wild. I once split a scored venlafaxine tablet because it ‘looked like it was meant to.’ My pharmacist nearly fainted. Never again.
Siobhan K.
December 21, 2025 AT 11:04Let me guess-you crushed your ER pill because you were impatient and then blamed the drug for not working fast enough. Classic. The fact that people still think scored lines mean ‘safe to split’ is why we have ER overdose stats. Pharmacists aren’t magicians. They can’t fix dumb decisions. Stop assuming your intuition beats pharmaceutical engineering.
Jerry Peterson
December 21, 2025 AT 13:32Man, I used to take Adderall IR for focus-then switched to XR after my doc explained the peaks and crashes. Life changed. No more 3 p.m. zombie mode. But I still keep a 5 mg IR on hand for big presentations. It’s like having a turbo button. Just don’t mash it all day. And yeah-never crush anything. Learned that the hard way after a friend ended up in the ER. Not worth it.
Meina Taiwo
December 23, 2025 AT 12:54ER pills take time. Don’t skip doses. Don’t crush them. Simple.
Southern NH Pagan Pride
December 24, 2025 AT 21:54Wait… so the FDA says ER meds are safe? LOL. Have you seen how many of these are made by Big Pharma? They design them to be ‘tamper-resistant’ because they know people will abuse them. The real danger? The system wants you dependent on slow-release drugs so you keep buying them. And the score lines? That’s a trap. They put them there to make you feel like you’re in control… but you’re not. You’re just another data point in their profit chart.
Swapneel Mehta
December 26, 2025 AT 06:06This is actually one of the most useful posts I’ve read in months. I’ve been on bupropion XL for anxiety and thought it wasn’t working after five days. Turned out I just needed patience. Also, the part about gastroparesis? My uncle has that and was on ER metoprolol-ended up in ICU. Never thought to connect the dots. Thanks for the clarity. Sharing this with my family.
Cameron Hoover
December 26, 2025 AT 19:32I used to be the guy who’d crush his Adderall XR because ‘I need it NOW.’ Then I had a panic attack that felt like my heart was trying to escape my chest. Turns out, 30 mg of immediate-release stimulant in 20 seconds? Bad idea. I’m now a full-on ER evangelist. No more shortcuts. No more ‘I’ll just split it.’ I treat these pills like they’re made of glass. Because they are.
Jay lawch
December 28, 2025 AT 14:58Let me tell you something about the pharmaceutical-industrial complex. These extended-release formulations? They’re not about your health-they’re about corporate control. Why? Because if you take a pill once a day, you’re more likely to stay dependent. The system doesn’t want you cured. It wants you compliant. The ‘steady levels’ narrative? A distraction. The real goal is to keep you on the treadmill of monthly prescriptions. And don’t get me started on how they patent minor coating changes to extend monopolies. This isn’t medicine. It’s capitalism with a stethoscope.
Christina Weber
December 29, 2025 AT 15:27There is a critical error in your post. You state that ‘92% of ER formulations can’t be safely altered.’ That is an imprecise statistical claim without a cited source. Additionally, you use ‘ER’ and ‘XR’ interchangeably, which is misleading-XR denotes extended-release, but SR and CR have distinct release mechanisms. Furthermore, your assertion that ‘pharmacists report 23% of medication errors’ lacks institutional attribution. As a licensed clinician, I must insist on data integrity. Please revise and cite your sources before disseminating medical advice.
Michael Ochieng
December 30, 2025 AT 06:50Love this breakdown. I’m Nigerian-American and my mom still thinks if a pill is big, you gotta split it ‘to make it easier.’ I had to sit her down with a bottle of metformin XR and show her the coating. She’s now the family pill police. Also, the cost thing? Yeah, ER is pricier-but I’ve saved $1,200 in ER visits since switching. Worth every penny. And no, you can’t just ‘take two IRs’ to match an ER. That’s how people end up on TikTok with ‘I crushed my pill and now I’m a zombie’ videos.
Dan Adkins
December 31, 2025 AT 08:17It is imperative to note that the structural integrity of extended-release pharmaceutical formulations is predicated upon proprietary matrix systems that are not amenable to mechanical alteration. Any deviation from the prescribed administration protocol constitutes a pharmacokinetic violation of the intended therapeutic paradigm. The assertion that patients may ‘feel’ the medication’s efficacy within 30 minutes is not only empirically unsound but also indicative of a profound misunderstanding of pharmacodynamic principles. I urge all individuals to consult the manufacturer’s prescribing information prior to any modification of dosage form. Failure to do so may result in catastrophic systemic toxicity.