Every year, over 100,000 people in the U.S. die from adverse drug reactions - and heart medications are at the center of many of these tragedies. It’s not always the drugs themselves that kill. It’s what happens when you mix them. A simple over-the-counter painkiller, a supplement you think is harmless, or even a glass of wine can turn a life-saving heart pill into a silent killer. You’re not alone if you didn’t know this. Most patients don’t. And doctors, even when they mean well, often miss these deadly combinations during busy appointments.
Why Heart Medications Are Especially Risky
Your heart doesn’t just beat - it responds to every chemical in your body. Medications that control blood pressure, rhythm, or fluid levels work with extreme precision. Even small changes in how these drugs interact can throw your entire system off balance. Unlike antibiotics or allergy meds, heart drugs often have narrow safety margins. A little too much of one can cause your blood pressure to crash. A little too little of another can let a clot form. And when two or more are mixed, the effects aren’t just added - they multiply.A 2023 study from the USC Schaeffer Center tracked nearly 10,000 older adults taking multiple medications. Those on just one heart drug with known cardiovascular risks had a 35% higher chance of a heart attack or stroke. Those on three? Risk jumped 218%. That’s not a typo. Three medications - each prescribed for a separate condition - nearly tripled the danger.
The 7 Deadliest Combinations You Must Know
These aren’t theoretical risks. These are real, documented, and deadly. If you take any of these, you need to talk to your doctor today.- Warfarin + Ibuprofen: Warfarin thins your blood. Ibuprofen irritates your stomach lining. Together, they increase your risk of a life-threatening gastrointestinal bleed by 300%. One study found patients on this combo had INR levels spike unpredictably, leading to emergency hospitalizations after minor injuries or dental work.
- Warfarin + Acetaminophen: You might think Tylenol is safe. But when taken regularly with warfarin, it can raise your INR by 2 to 3 points - enough to cause internal bleeding. This isn’t a one-time thing. It builds up over weeks.
- PDE-5 inhibitors (Viagra, Cialis) + Nitrates: This combo can drop your systolic blood pressure below 70 mmHg. That’s lower than what many people have during cardiac arrest. The result? Sudden collapse, stroke, or death. Even one dose of a nitrate patch or spray can trigger this if you’ve taken a PDE-5 inhibitor in the last 48 hours.
- Statins + Amiodarone: Amiodarone, used for irregular heartbeats, slows how your body clears statins. This can cause muscle breakdown (rhabdomyolysis), which leads to kidney failure. The risk jumps 400-500%. Many patients don’t know they’re on both until it’s too late.
- ACE inhibitors + Potassium supplements: ACE drugs like lisinopril help your heart by lowering blood pressure - but they also cause your body to hold onto potassium. Add a potassium pill or salt substitute, and your levels can soar past 5.5 mEq/L. At that point, your heart can suddenly stop beating. One 2021 study found 18.7% of patients on this combo developed dangerous hyperkalemia - compared to just 4.2% who weren’t.
- Digoxin + Verapamil: Verapamil, a calcium channel blocker, blocks the kidneys from clearing digoxin. Serum digoxin levels can rise 60-75%. That’s enough to cause nausea, confusion, visual disturbances, and fatal arrhythmias. Many older adults take both - one for heart failure, one for atrial fibrillation - without realizing the danger.
- NSAIDs (Diclofenac, Indomethacin, Ketorolac) + Any Blood Pressure Med: NSAIDs don’t just hurt your stomach. They make your kidneys hold onto salt and water, which raises blood pressure. They also cut the effectiveness of diuretics by 25-30%. For someone with heart failure, this can mean sudden fluid overload, hospitalization, or death. Over 70 million NSAID prescriptions are written every year in the U.S. - and most patients have no idea they’re sabotaging their heart meds.
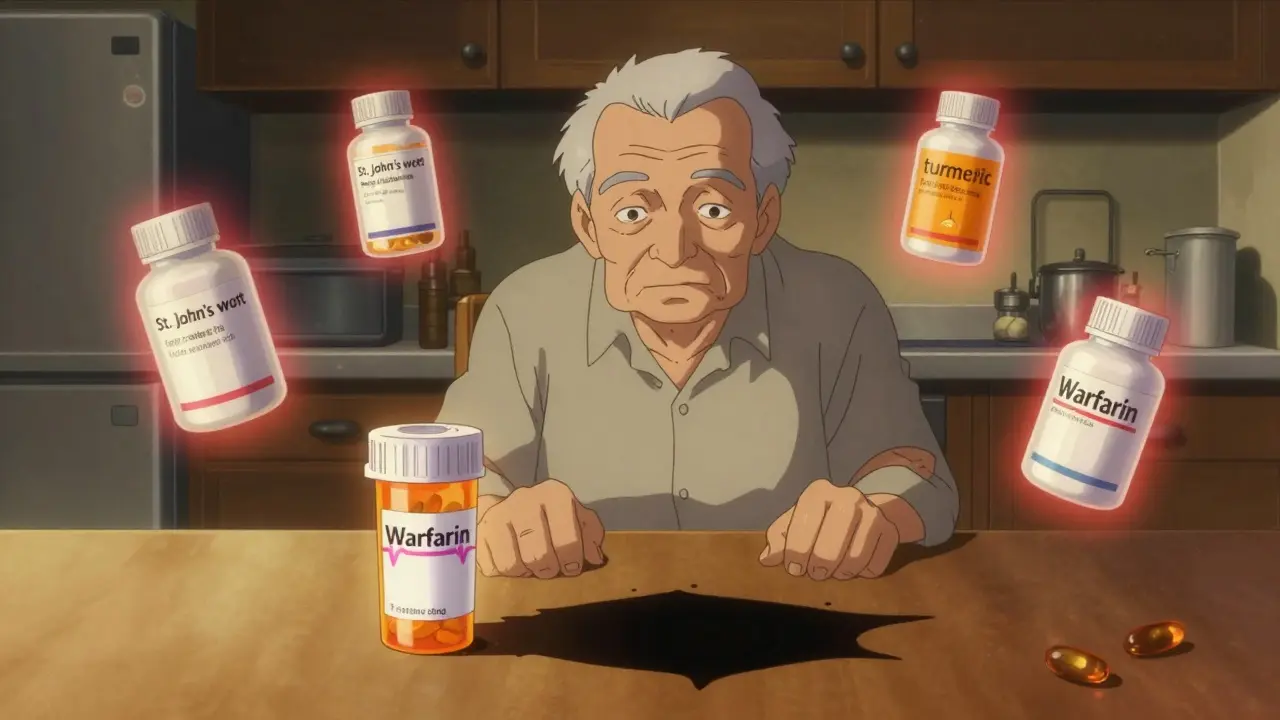
What About Supplements? You’re Probably Taking One
You think herbal stuff is safe because it’s “natural.” That’s the biggest mistake.St. John’s wort - commonly taken for depression - cuts the blood levels of warfarin by up to 50%. That means your blood gets thicker. You’re at higher risk for stroke or heart attack. Turmeric, ginger, garlic, and ginkgo biloba all thin the blood. Take them with warfarin, aspirin, or clopidogrel, and you’re playing Russian roulette with bleeding.
Even magnesium supplements can be dangerous if you’re on certain heart drugs. Too much can slow your heart rate or cause low blood pressure - especially if you have kidney problems. And don’t assume your pharmacist knows. Most don’t track supplements unless you tell them.
What’s Actually Safe?
Not all combinations are bad. Some are lifesavers.Statins, aspirin, and beta-blockers together reduce death risk by 25-30% in high-risk patients. SGLT2 inhibitors like dapagliflozin - when added to standard heart failure meds - cut cardiovascular events by 14%. These aren’t accidents. They’re science-backed, carefully studied combinations designed to work together.
The key difference? These were tested in clinical trials. The dangerous ones? They’re the ones doctors didn’t test - because they’re not supposed to be taken together.
What You Can Do Right Now
You don’t need to be a medical expert to protect yourself. Just follow these steps:- Make a complete list: Write down every pill, patch, vitamin, herb, and OTC drug you take - including doses and how often. Don’t say “blood pressure pill.” Say “lisinopril 10 mg once daily.”
- Bring it to every appointment: Even if you’ve seen your doctor before. Give it to the nurse, the pharmacist, and the doctor. Ask: “Could any of these interact with each other?”
- Use one pharmacy: Chain pharmacies like CVS or Walgreens can flag dangerous combinations. If you use three different pharmacies, you’re flying blind.
- Ask about new meds: When your doctor prescribes something new, ask: “Is this safe with what I’m already taking?” Don’t wait for them to bring it up.
- Check your OTC meds: Read labels. If it says “may interact with heart medications,” stop taking it until you talk to your doctor.
Medicare Part D now covers 30-minute medication reviews with pharmacists - free of charge. Use it. If your doctor doesn’t offer this, ask for a referral. It’s your right.

Why This Keeps Happening
The system is broken. In 2023, only 37% of primary care doctors routinely screen for dangerous combinations. Most don’t have time. Electronic systems flag some risks - but not all. They often miss supplements, OTC drugs, or older combinations that haven’t been updated in the database.Patients are left guessing. A 2022 survey found 62% of heart failure patients weren’t warned about dangerous interactions. On Reddit, 78% of users reported side effects from mixing meds. One woman shared how she took ibuprofen for a headache, didn’t tell her cardiologist, and ended up in the ER with a GI bleed. Another took St. John’s wort with warfarin and had an INR of 8.0 - nearly fatal.
It’s not about being careless. It’s about being uninformed. And that’s fixable.
The Future Is Getting Better - But Not Fast Enough
New tools are coming. AstraZeneca just launched a single pill combining three proven heart failure drugs - reducing the chance of bad interactions by simplifying the regimen. AI-powered screening tools are being tested and could cut dangerous combinations by half in the next five years. The FDA now requires black box warnings on NSAIDs for patients on anticoagulants.But none of that helps you today. The only thing that will is you - knowing what to ask, what to check, and what to avoid.
Can I take ibuprofen if I’m on a blood thinner?
No. Ibuprofen and other NSAIDs increase the risk of severe bleeding by 300% when taken with warfarin, apixaban, rivaroxaban, or aspirin. Even occasional use can trigger a dangerous bleed. Use acetaminophen instead - but only if you’re not on long-term warfarin. Always check with your doctor first.
Is it safe to take turmeric or fish oil with heart meds?
Turmeric, fish oil, garlic, and ginger all have blood-thinning effects. If you’re on warfarin, clopidogrel, or aspirin, they can increase your bleeding risk. A single high-dose fish oil supplement (over 3 grams daily) can interfere with clotting. Talk to your doctor before taking any supplement - even if it’s labeled “natural.”
What should I do if I accidentally took a dangerous combo?
Call your doctor or pharmacist immediately. If you feel dizzy, weak, have chest pain, notice unusual bruising or bleeding, or have dark, tarry stools - go to the ER. Don’t wait. Some interactions cause damage within hours. Others build up over days. Either way, time matters.
Can my pharmacist check for dangerous interactions?
Yes - and Medicare Part D pays for it. Ask for a Medication Therapy Management (MTM) session. It’s a free 20-30 minute review where the pharmacist looks at every pill, supplement, and OTC drug you take. They’ll flag risks you didn’t know about. Bring your full list - and don’t leave without a printed summary.
Why don’t doctors warn me about these combinations?
Many don’t know. Others assume you’re taking only what’s prescribed. They don’t ask about supplements, OTC drugs, or what you’re taking for a cold. In 2023, only 37% of primary care doctors routinely screen for dangerous interactions. You have to be your own advocate. Ask. Bring your list. Push for clarity.
Are there any heart meds that are safe to mix?
Yes - but only the ones proven in studies. Statins, aspirin, and beta-blockers together reduce death risk by 25-30%. SGLT2 inhibitors like dapagliflozin, when added to standard heart failure treatment, reduce hospitalizations by 14%. These are carefully tested combinations. Never assume a new mix is safe just because it seems logical. Always check.