More than half of U.S. adults take herbal supplements. Many believe they’re safe because they’re "natural." But what they don’t realize is that these same supplements can turn life-saving medications into useless pills-or worse, trigger dangerous side effects. If you’re on blood thinners, antidepressants, or heart meds, your daily turmeric capsule or ginkgo tablet could be putting you at risk.
St. John’s Wort: The Silent Medication Killer
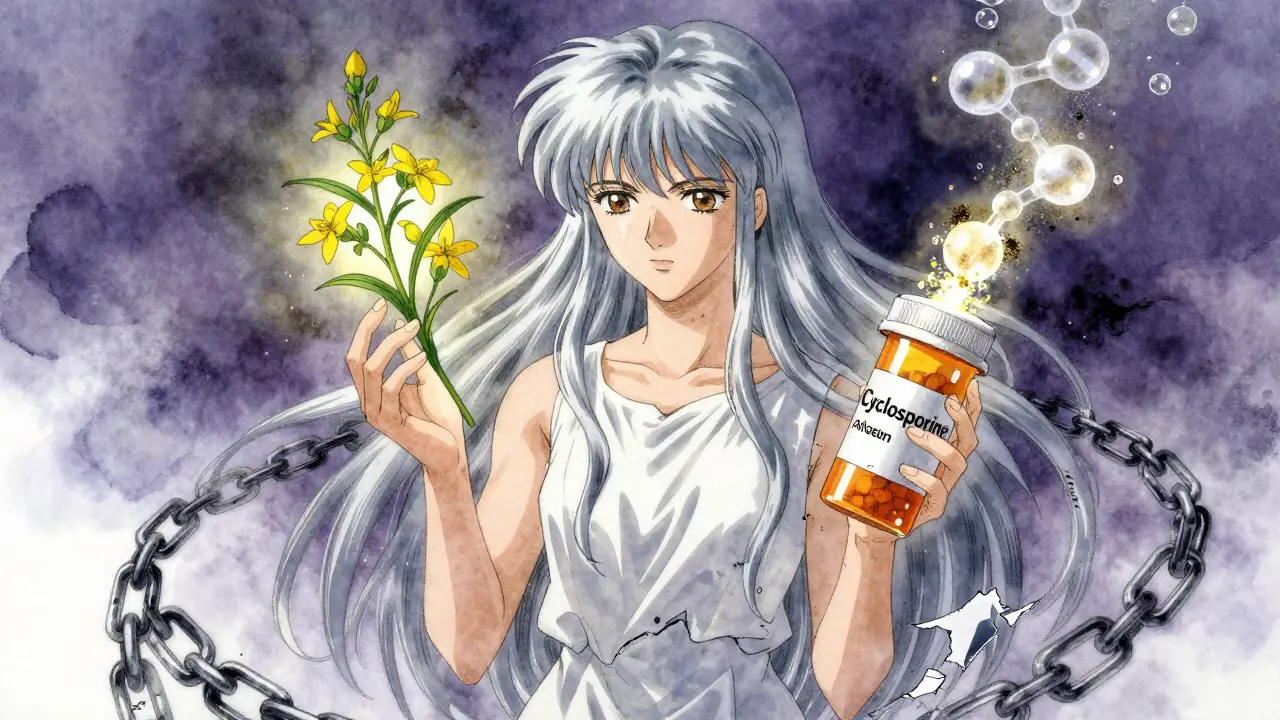
St. John’s Wort is one of the most popular herbal mood boosters. It’s in teas, capsules, and gummies marketed for anxiety and mild depression. But here’s the problem: it doesn’t just affect your mood-it affects how your body handles nearly every prescription drug you take.
This herb activates an enzyme in your liver called CYP3A4, which speeds up how fast your body breaks down medications. The result? Drugs like cyclosporine (for organ transplants), birth control pills, and HIV medications get flushed out before they can work. A 2021 review by the National Center for Complementary and Integrative Health found St. John’s Wort cuts cyclosporine levels by 50-60%. That’s not a minor drop-it’s enough to cause organ rejection.
It doesn’t stop there. When taken with SSRIs like sertraline or fluoxetine, St. John’s Wort can trigger serotonin syndrome. Symptoms include high fever, muscle stiffness, confusion, and rapid heartbeat. In severe cases, it’s fatal. The American Academy of Family Physicians warns: "Avoid St. John’s Wort entirely if you’re on any antidepressant." And yet, 78% of users on Drugs.com forums didn’t know this until they had a bad reaction-some even got pregnant while on birth control because the herb made it ineffective.
Ginkgo Biloba: The Hidden Bleeding Risk
Ginkgo is sold as a memory enhancer, brain booster, or circulation aid. It’s in 73% of all "brain health" supplements, according to ConsumerLab’s 2022 testing. But if you’re on warfarin, apixaban, or even aspirin, you’re playing Russian roulette with your blood.
Studies from the Mayo Clinic show 23 documented cases of major bleeding between 2010 and 2020 linked to ginkgo and blood thinners. Three of those cases ended in death. The herb interferes with platelet function and increases bleeding time. One Reddit user, u/HeartPatient99, shared how his INR spiked to 8.2 after combining ginkgo with apixaban. He ended up in the ER with severe rectal bleeding. His doctors said this happens more often than people admit.
Even if you’re not on a strong blood thinner, ginkgo can still be risky. A 2019 meta-analysis found it increases bleeding risk by 300% compared to warfarin alone. And there’s no safe dose. If you’re taking it, stop before surgery-ideally, at least two weeks ahead. But most people don’t tell their surgeon they’re taking it. That’s the real danger.
Garlic: More Than Just a Flavor
Garlic supplements are popular for immune support and heart health. But if you’re on blood thinners or HIV drugs like saquinavir, garlic can be dangerous. A 2019 University of Washington trial with 18 healthy volunteers showed garlic reduced saquinavir levels by 51%. That’s a massive drop-enough to let the virus rebound.
Garlic also thins the blood. While eating garlic in food is fine, concentrated supplements (capsules, extracts) have measurable effects. A 2019 study in the Journal of Clinical Pharmacy and Therapeutics found that garlic combined with warfarin increased bleeding risk by 40%. And like ginkgo, it’s rarely disclosed. In a Stony Brook Medicine study of over 5,000 Medicare patients, nearly 300 reported risky combinations involving garlic, ginkgo, or ginseng with blood thinners.

Goldenseal: The Enzyme Blocker
Goldenseal is often marketed as a cold remedy or immune booster. But its real power lies in how it blocks liver enzymes. It inhibits CYP3A4-the same enzyme St. John’s Wort activates. That means it can make drugs stick around too long, increasing toxicity.
A 2018 University of Toronto study showed goldenseal reduced midazolam clearance by 40%. Midazolam is a sedative used before surgery. If you take goldenseal and then get put under anesthesia, you could overdose on the drug because your body can’t clear it. The same risk applies to statins, certain painkillers, and immunosuppressants.
Unlike St. John’s Wort, goldenseal doesn’t get much attention. But it’s in 12% of "immune support" blends. And because it’s sold as a "natural cold cure," people don’t think twice about taking it with their prescriptions.
Coenzyme Q10 and Ginseng: The Quiet Saboteurs
CoQ10 is promoted for heart health and energy. But if you’re on warfarin, it can make your blood thinner less effective. Mayo Clinic’s 2022 analysis found CoQ10 reduces warfarin’s anticoagulant effect by 25-30%. That means your INR drops. You might not feel anything-until you start bleeding internally.
Ginseng is trickier. Asian ginseng can lower blood sugar, which is dangerous if you’re on diabetes meds. It can also interfere with blood pressure drugs. A 2023 NCCIH summary noted some studies show ginseng reduces systolic blood pressure by 10-15 mmHg on top of medication. That’s enough to cause dizziness, fainting, or falls in older adults.
And then there’s the serotonin risk. Ginseng combined with MAO inhibitors (used for depression) can trigger serotonin syndrome. It’s rare-but when it happens, it’s life-threatening.
What About Cranberry and Milk Thistle?
Not all herbs are high-risk. Cranberry juice is often blamed for interacting with warfarin, but the evidence is mixed. A 2020 JAMA meta-analysis of 12 studies showed inconsistent INR changes-some patients had spikes, others didn’t. The FDA doesn’t list cranberry as a high-risk interaction. Still, if you’re on warfarin, stick to small amounts and monitor your INR.
Milk thistle and saw palmetto are generally considered low-risk. They don’t significantly affect liver enzymes or drug metabolism. Black cohosh is also low-risk for most people. But "low-risk" doesn’t mean "no risk." Always check with your doctor before starting anything.

How to Protect Yourself
Here’s the hard truth: your doctor probably doesn’t ask about supplements. Most don’t have time. And most patients don’t think it’s important to mention.
But you need to change that. At every doctor’s visit, say this: "I’m taking these supplements-here’s the list." Write them down. Include brand names, doses, and how often you take them. Don’t say "I take ginkgo for memory." Say: "I take 120 mg of ginkgo biloba daily."
Use the NCCIH Herb-Drug Interaction Checker. It’s free, updated quarterly, and classifies interactions as life-threatening, significant, or moderate. If your supplement is on the list, talk to your pharmacist. They’re trained to spot these conflicts.
Watch for warning signs: unexplained bruising, nosebleeds, dizziness, confusion, rapid heartbeat, or sudden changes in mood. If you’re on warfarin and your INR jumps above 4.0, call your doctor immediately. If you’re on antidepressants and feel agitated or feverish, don’t wait-go to the ER.
The Bigger Problem: No Regulation
The Dietary Supplement Health and Education Act of 1994 says supplements don’t need FDA approval before sale. That means companies can put anything in them-except drugs. But many do anyway. In 2022, the FDA warned 17 companies for slipping synthetic antidepressants and steroids into "natural" products.
There are no standardized labels. One brand’s "ginkgo" might have 50 mg; another’s might have 200 mg. And there’s no requirement to test for interactions. So you’re trusting a label that might be wrong.
That’s why you can’t rely on marketing claims. You can’t assume "natural" means safe. You can’t assume your doctor knows. You have to be your own advocate.
Bottom Line
Herbal supplements aren’t harmless. They’re powerful. And when mixed with prescription drugs, they can turn routine care into a medical emergency. St. John’s Wort, ginkgo, garlic, and goldenseal are the biggest culprits. But even "safe" herbs like CoQ10 and ginseng can interfere with your meds.
If you’re on any prescription drug, don’t start a supplement without talking to your doctor or pharmacist. And if you’re already taking one, don’t wait for symptoms. Get checked now. Your life might depend on it.

Jane Wei
December 16, 2025 AT 21:12I took St. John’s Wort for three months last year thinking it was just a "natural mood boost." Didn’t realize it was nuking my birth control until I got pregnant. My OB literally yelled at me. Don’t be me.
Naomi Lopez
December 17, 2025 AT 02:31It’s astonishing how many people still treat herbal supplements like tea leaves in a mug. The pharmacokinetic interactions are not theoretical-they’re documented, peer-reviewed, and lethal. If you’re on warfarin and popping ginkgo, you’re not being holistic-you’re being reckless. The FDA doesn’t regulate these because they’re not drugs, but that doesn’t make them safe. It makes them unregulated poisons with marketing budgets.
Martin Spedding
December 18, 2025 AT 20:32st johns wort is the worst. i took it with zoloft and woke up feeling like my brain was melting. ER. 4 hours. $8k bill. never again. also why is garlic even in this list? it’s just garlic.
Raven C
December 19, 2025 AT 20:35One cannot help but observe the profound societal disregard for biochemical integrity in the pursuit of pseudo-scientific wellness. The normalization of unregulated phytochemical consumption-especially when paired with life-sustaining pharmaceuticals-is not merely irresponsible; it is a systemic failure of public health education. I weep for the future.
Donna Packard
December 20, 2025 AT 17:00I’m so glad someone wrote this. My mom had a scary bleed last year after taking ginkgo with her blood thinner. She didn’t even know it could do that. Please, if you’re reading this-talk to your pharmacist. They’re the real heroes.
Patrick A. Ck. Trip
December 21, 2025 AT 03:25good post. i think more peopel need to know this. i used to take coq10 with warfarin cause i read online it was 'good for heart'. turns out it made my inr drop to 1.8. scary stuff. i stopped. now i just eat salmon.
Jessica Salgado
December 22, 2025 AT 06:45Okay but why is no one talking about how supplement labels are often completely wrong? I bought a "100% pure ginkgo biloba" capsule that had 200mg of ginkgo, but the bottle said 120mg. And the third one I bought had a different extract ratio entirely. There’s no standardization. It’s like playing Russian roulette with your liver.
Steven Lavoie
December 23, 2025 AT 01:49As someone who grew up in a household where every ailment was treated with herbs-turmeric for inflammation, ashwagandha for stress-I’m grateful this was written. But I also know how hard it is to shift cultural habits. My grandmother still swears by garlic for high blood pressure. The key isn’t to shame-it’s to educate with compassion. Talk to your elders. Show them the studies. They just want to feel safe.
Michael Whitaker
December 24, 2025 AT 00:13Let me just say this: if you’re taking supplements, you’re either a) ignorant, b) gullible, or c) paying for placebo. The fact that you think "natural" means "safe" is the exact reason pharmaceutical companies don’t have to warn you. You’re the perfect customer. Wake up.
Jigar shah
December 25, 2025 AT 19:19Interesting article. I take ashwagandha and metformin in India. Is there any known interaction? I’ve never heard of any, but I’m curious. Maybe someone can share experience?
Marie Mee
December 27, 2025 AT 00:51the government and big pharma are hiding this. they dont want you to know herbs are better than drugs. they make more money off pills. st johns wort cures depression better than antidepressants and they dont want you to know. its all a scam. the FDA is corrupt
Salome Perez
December 28, 2025 AT 19:38This is such an important piece-and I’m so glad you included the NCCIH checker. As a clinical pharmacist, I’ve seen too many patients come in with INRs off the charts or serotonin syndrome from "innocent" supplements. I always hand out a printed list of high-risk herbs with their med list. If you’re on meds, carry this list to every appointment. And yes, even milk thistle can interact with some antivirals-don’t assume "low-risk" means "no risk." You’re your own best advocate.
Josh Potter
December 30, 2025 AT 18:27bro i took garlic pills for my cholesterol and then my knee started bleeding out after a minor injury. doc said it was the garlic + aspirin combo. i thought i was being healthy. turned out i was being dumb. now i just eat actual garlic. no pills. life is better.
Evelyn Vélez Mejía
December 31, 2025 AT 20:48The philosophical underpinning of this discourse reveals a deeper epistemological crisis in modern healthcare: the conflation of tradition with evidence, and the romanticization of nature as inherently benign. The Cartesian dualism between "natural" and "synthetic" is not merely misleading-it is dangerously reductive. To treat herbal compounds as exempt from pharmacological scrutiny is to abandon the very principles of empirical medicine that have saved millions. This is not anti-alternative medicine; it is pro-scientific rigor.
Nishant Desae
January 2, 2026 AT 11:39I’ve been taking ginseng for years to help with energy, especially since I work night shifts. I also take lisinopril for blood pressure. I didn’t realize it might lower it too much until I passed out at the grocery store last winter. My wife found me on the floor. Turns out, ginseng + blood pressure meds = dizziness city. I stopped it, and now I just drink green tea and take walks. My BP’s stable. I’m so glad I didn’t wait for something worse to happen. If you’re on meds, don’t guess-ask your pharmacist. They’ll help you, no judgment. Seriously.