Teens are growing up fast. One day they’re asking you to help them find their inhaler before soccer practice; the next, they’re packing for college and you’re wondering if they’ll remember to take their ADHD meds-or worse, if they’ll share them with a friend. Teaching teens to manage their own prescription medications isn’t just a chore. It’s a life skill that can prevent overdose, addiction, and long-term health problems. And it’s not something you wait until they leave home to start. The clock starts ticking in 10th grade.
Start with Understanding, Not Just Instructions
Most teens don’t know why they’re taking their meds. They just know they’re supposed to. That’s dangerous. A 2020 DEA report found that 70% of teens think prescription drugs are safer than street drugs. That’s not just ignorance-it’s a ticking time bomb. Sit down with your teen and go through every pill, patch, or inhaler they use. Don’t assume they know what it’s for. Ask them: "What does this do?" If they can’t answer, explain it in plain terms. Don’t say "it regulates neurotransmitters." Say: "This helps you focus in class so you don’t zone out during lectures." Or: "This stops your asthma from flaring up when you run." Make sure they know the risks too. If they’re on opioids for pain, tell them: "Taking more than prescribed can stop your breathing. Sharing it can kill someone." If it’s an ADHD med, explain: "This isn’t a study drug. Taking it without a prescription can raise your blood pressure and cause heart problems." Facts stick better than fear.Build a Routine That Sticks
Teens don’t think like adults. They don’t wake up thinking, "I need to take my meds." They think, "I need to get to school on time." That’s why tying meds to existing habits works. Research from the University of Rochester shows teens who link medication to daily routines like brushing teeth or eating breakfast are 37% more likely to take them on time. So if your teen takes their antidepressant at night, make it part of their bedtime ritual: "Brush teeth, wash face, take pill, turn off light." If it’s a morning med, pair it with grabbing their backpack or pouring cereal. Use alarms. Not just one. Set three: 10 minutes before, at the exact time, and 15 minutes after. A 2020 University of Michigan study found that multiple reminders boosted teen adherence by 41%. Use their phone. Most teens never leave it behind. Apps like Medisafe or MyMeds can send notifications, track doses, and even alert you if they miss one. But don’t just install it-use it together. Practice setting up the alarms. Test the alerts. Make sure it’s not silenced during class.Use Tools That Actually Work
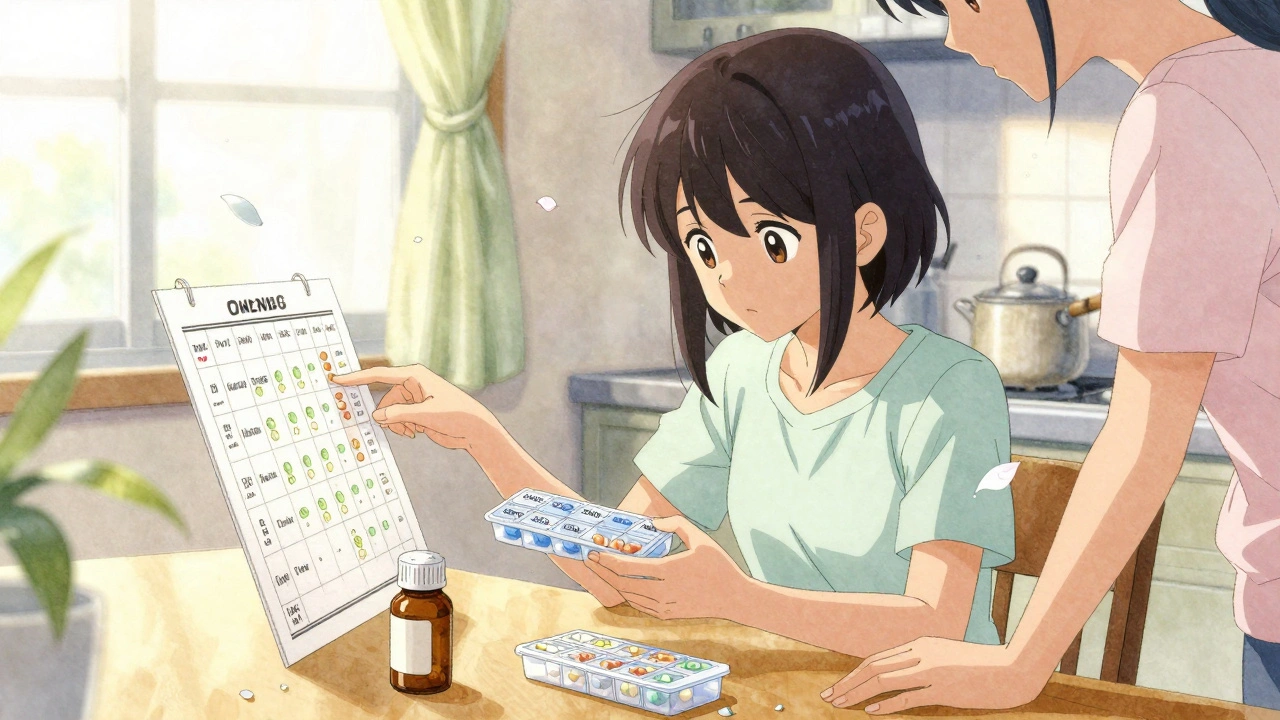
A pill organizer isn’t just for grandparents. It’s a game-changer for teens. Get one with separate compartments for morning, afternoon, evening, and weekend doses. Label it clearly. Let your teen pick the color or design-ownership matters. For complex regimens, try a weekly tracker. Print a simple chart with boxes for each day and time. Have them check off doses as they take them. It’s visual, satisfying, and gives you a quick way to spot missed doses without nagging. Digital tools help-but not all apps are created equal. A 2023 Mayo Clinic review found only 22% of teen medication apps have been clinically tested. Stick with ones recommended by your pharmacist or pediatrician. Avoid apps that just remind you-they need to log intake, track side effects, and sync with your phone’s health data.Gradually Hand Over Control
You can’t hand over the keys to the car without a driver’s ed class. Same with meds. Don’t go from full supervision to "good luck" overnight. Start in 10th grade: Let them identify their meds and describe their purpose. In 11th grade, let them refill prescriptions with your help. Show them how to call the pharmacy, check dosage, and ask about interactions. By 12th grade, they should be able to request refills, schedule appointments with their doctor, and report side effects on their own. Use a step-by-step transition:- Parent administers all meds
- Parent sets alarms, teen takes pill
- Teen sets alarms, parent texts to confirm
- Teen takes meds, logs in app, parent checks weekly
- Teen manages everything, parent does random spot-checks

Controlled Substances Need Extra Rules
Painkillers, anxiety meds, and ADHD drugs are the most commonly misused by teens. The DEA says they’re the second most popular illicit drug after marijuana. And they’re often just sitting in your medicine cabinet. Lock them up. Use a small lockbox-something you can keep on a shelf, not in the bathroom. Only give your teen access when they’re ready to take it. Count pills monthly. If you’re missing 3 oxycodone tablets, that’s not a mistake. That’s a red flag. Never let a teen manage opioids or benzodiazepines alone. Even if they’re responsible, the risk is too high. Dr. Harold Paz of Aetna says it plainly: "Even responsible teens should not be allowed to control their painkillers." That means you’re still the keeper of the keys-until they’re 18, in college, and have a pharmacy they trust.Teach Them How to Talk to Doctors
Teens often hide side effects because they’re scared of being told to stop their meds-or worse, being labeled "dramatic." They need to know how to speak up. Practice role-playing. You be the doctor. They’re the patient. Have them say: "I’ve been feeling dizzy after I take this. It happens every afternoon." Or: "I skipped a dose because I didn’t want to take it at lunch." Then switch roles. Show them how to ask: "Is there a lower dose? A different time to take it?" Encourage them to bring a list of questions to appointments. Write them down. Keep it simple: "What happens if I miss a day?" "Can I take this with energy drinks?" "Are there any foods I should avoid?"" The more they practice, the less intimidating it becomes. And when they can speak for themselves, they’re less likely to hide problems.Peer Support Makes a Difference
Teens listen to friends more than parents. That’s why having a medication buddy helps. Find another teen who takes daily meds-maybe a classmate with asthma or diabetes. Encourage them to check in with each other. Not to compare, but to share reminders: "Hey, did you take your pill today?" Research in the Journal of Adolescent Health shows teens with a medication partner are 22% more likely to stay on track. Schools are catching on too. Programs like Generation Rx’s "My Generation Rx" teach teens how to say no to peer pressure around pills. Schools that use it report 33% fewer cases of prescription misuse. Ask your school if they offer it. If not, suggest it.
Dispose of Unused Meds Properly
Old antibiotics from last winter? Unused painkillers from a sports injury? Don’t keep them. Don’t flush them. Don’t toss them in the trash. The DEA runs over 14,000 drug take-back locations across the U.S.-pharmacies, police stations, hospitals. Find one near you. Drop off unused meds. It’s free, safe, and stops someone else from grabbing them. If you can’t get to a drop-off, mix pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. It makes them unappealing and unusable.What If They Still Forget?
Mistakes happen. A teen misses a dose. They skip a week. They take two by accident. Don’t panic. Don’t punish. Call their doctor. Ask: "What should we do if they miss a dose?" Some meds are fine to take late. Others aren’t. Get the protocol in writing. Use it as a learning moment. Ask: "What made you forget?" Was it a late night? A change in schedule? A party? Then adjust the system. Maybe they need a louder alarm. Maybe they need to carry a small pill case in their backpack. The goal isn’t perfection. It’s progress.What’s Next?
By the time they’re 18, they should be able to:- Identify every medication they take and why
- Set and manage their own reminders
- Request refills and talk to pharmacists
- Report side effects to their doctor
- Store meds safely and dispose of them properly
- Say no to peers asking for pills
Medication management isn’t a one-time lesson. It’s a practice. You’re not teaching them to follow rules-you’re teaching them to care for themselves. And that’s the most important prescription of all.
At what age should I start teaching my teen to manage their meds?
Start in 10th grade. That’s when teens begin to need more independence, and it gives them time to build skills before college. The American Academy of Pediatrics recommends beginning with basic understanding-what the meds are for and how to read labels-then gradually increasing responsibility through 11th and 12th grade.
Can I let my teen manage their own painkillers?
No. Even responsible teens should not manage opioids or other controlled pain medications alone. These drugs carry a high risk of misuse and overdose. Store them in a locked box, count them monthly, and only hand them out as needed. The American Academy of Pediatrics and Aetna both recommend parental control over these medications until the teen is fully independent and in a controlled environment like college with access to a pharmacy.
What apps are best for teens managing meds?
Stick with apps that have been clinically tested for teens, like Medisafe and MyMeds. Avoid random apps from the app store-only 22% of medication apps have been validated for adolescent use, according to Mayo Clinic’s 2023 review. Look for apps that let you log doses, send multiple reminders, and sync with your phone’s health data. Always test the app with your teen before relying on it.
How do I know if my teen is misusing their meds?
Watch for signs like missing pills, secretive behavior, mood swings, declining grades, or sudden changes in friends. If they’re on ADHD meds, watch for excessive energy, insomnia, or weight loss. If they’re on painkillers, watch for drowsiness, slurred speech, or frequent requests for refills. If you suspect misuse, don’t confront them angrily. Say: "I noticed you’ve been running out of your meds early. Can we talk about why?" Then contact their doctor.
What if my teen refuses to take their meds?
Don’t force them. Ask why. Sometimes it’s side effects. Sometimes it’s embarrassment. Sometimes they don’t believe it’s helping. Talk to their doctor about alternatives-different dosing times, different medications, or non-pill options like patches or liquids. Involve them in the decision. Teens are more likely to take meds they helped choose.
Should my teen carry their meds to school?
It depends on the medication and school policy. For daily meds like asthma inhalers or ADHD pills, yes-but only if the school allows it and has a plan in place. Many schools require meds to be stored in the nurse’s office. Talk to the school nurse and your teen’s doctor. If your teen needs to carry it, make sure they know how to store it safely and never share it. Keep a backup at home.
How often should I check on my teen’s meds?
Start with daily check-ins in 10th grade, then move to weekly text reminders in 11th grade, and monthly spot-checks by 12th grade. The goal is to reduce oversight as competence grows. Use apps that log doses so you can see patterns without constant questioning. If they’ve been consistent for three months, trust them-but keep the safety net of occasional checks.
Can my teen access their own medical records?
Yes. Under the 2020 CURES Act, teens as young as 13 can access their own electronic health records, including medication history, through patient portals. Encourage them to log in and review their prescriptions. It builds responsibility and helps them understand their own health. You can still be added as a family member to view records if you need to help manage them.

Maria Elisha
December 9, 2025 AT 11:17Lola Bchoudi
December 11, 2025 AT 03:34Carina M
December 11, 2025 AT 10:09Raja Herbal
December 12, 2025 AT 06:52Morgan Tait
December 13, 2025 AT 04:54Andrea Beilstein
December 14, 2025 AT 02:13Angela R. Cartes
December 15, 2025 AT 23:25om guru
December 16, 2025 AT 07:25Darcie Streeter-Oxland
December 18, 2025 AT 02:21Ryan Brady
December 19, 2025 AT 07:38