Take a pill that’s just a few months past its expiration date. For most medications, it’s probably fine. But for some, it could be life-threatening. If you’re taking a medication with a narrow therapeutic index, even a small drop in potency-or a slight change in how your body absorbs it-can push you from safe to dangerous in seconds. This isn’t theoretical. It’s happening in homes, hospitals, and nursing facilities across the U.S. every day.
What Exactly Is a Narrow Therapeutic Index?
A narrow therapeutic index (NTI) means there’s almost no room for error. The difference between a dose that works and a dose that harms is tiny. Think of it like walking a tightrope. One step too far left, and you fall into ineffective treatment. One step too far right, and you risk poisoning. The U.S. Food and Drug Administration defines NTI drugs as those where small changes in blood concentration can cause serious harm-like organ failure, uncontrolled seizures, or deadly blood clots. For most drugs, the gap between the minimum effective dose and the minimum toxic dose is wide. For NTI drugs, it’s often less than a twofold difference. That means if your blood level of the drug goes up just 50%, you could cross into toxicity. Examples? Warfarin, lithium, digoxin, phenytoin, levothyroxine, carbamazepine, and tacrolimus. These aren’t obscure drugs. They’re among the most commonly prescribed in the U.S. Warfarin prevents strokes in people with atrial fibrillation. Lithium stabilizes mood in bipolar disorder. Digoxin helps the heart pump more efficiently. Levothyroxine replaces thyroid hormone. Mess with any of these, and the consequences aren’t minor.Why Expiration Dates Matter More for NTI Drugs
Expiration dates aren’t arbitrary. They’re based on real-world testing. Manufacturers test how long a drug stays stable under normal storage conditions-temperature, humidity, light-and guarantee that it retains at least 90% of its labeled potency until that date. For most medications, losing 5% or 10% potency over time doesn’t matter much. But for NTI drugs, that 10% drop could be catastrophic. Take warfarin. Its therapeutic range is narrow: an INR of 2.0 to 3.0. If a patient’s INR drops below 2.0, they’re at risk of a stroke. If it climbs above 4.0, they could bleed internally. A 10% loss in warfarin potency could lower the INR by 0.5 to 1.0 units. That’s enough to push someone out of the safe zone. Digoxin is even more unforgiving. The therapeutic range is 0.5 to 0.9 nanograms per milliliter. Toxicity starts at 1.2. That’s only a 33% increase from the top of the safe range to the danger zone. If an expired digoxin tablet degrades and delivers 15% less drug, the patient might feel fine-until their heart rhythm starts to go haywire. No warning. No symptoms until it’s too late. And it’s not just about potency. Some drugs break down into harmful compounds. Tetracycline, though not an NTI drug, turns toxic when expired. While no NTI drug is known to produce deadly breakdown products, the risk isn’t zero. And with NTI drugs, you can’t afford to take chances.Generic Substitutions and the Hidden Risk
The FDA tightened bioequivalence standards for NTI drugs in 2011. Before that, generic versions had to be within 80% to 125% of the brand-name drug’s absorption. For NTI drugs, that’s way too wide. Now, for drugs like levothyroxine and phenytoin, the acceptable range is 90% to 111%. That’s a much tighter margin. But here’s the catch: even that 11% margin is tight. If a generic levothyroxine tablet is 10% less potent than the brand, and the patient has been stable on the brand for months, switching could cause their thyroid levels to swing. They might gain weight, feel fatigued, or develop heart rhythm problems-all because of a tiny change in dose. Now imagine that same generic tablet is six months past its expiration date. It’s already lost 5% potency. Now it’s 15% below what it should be. That’s outside the FDA’s own safety standard. Yet, patients take it anyway. Why? Because they think “it’s just a pill.”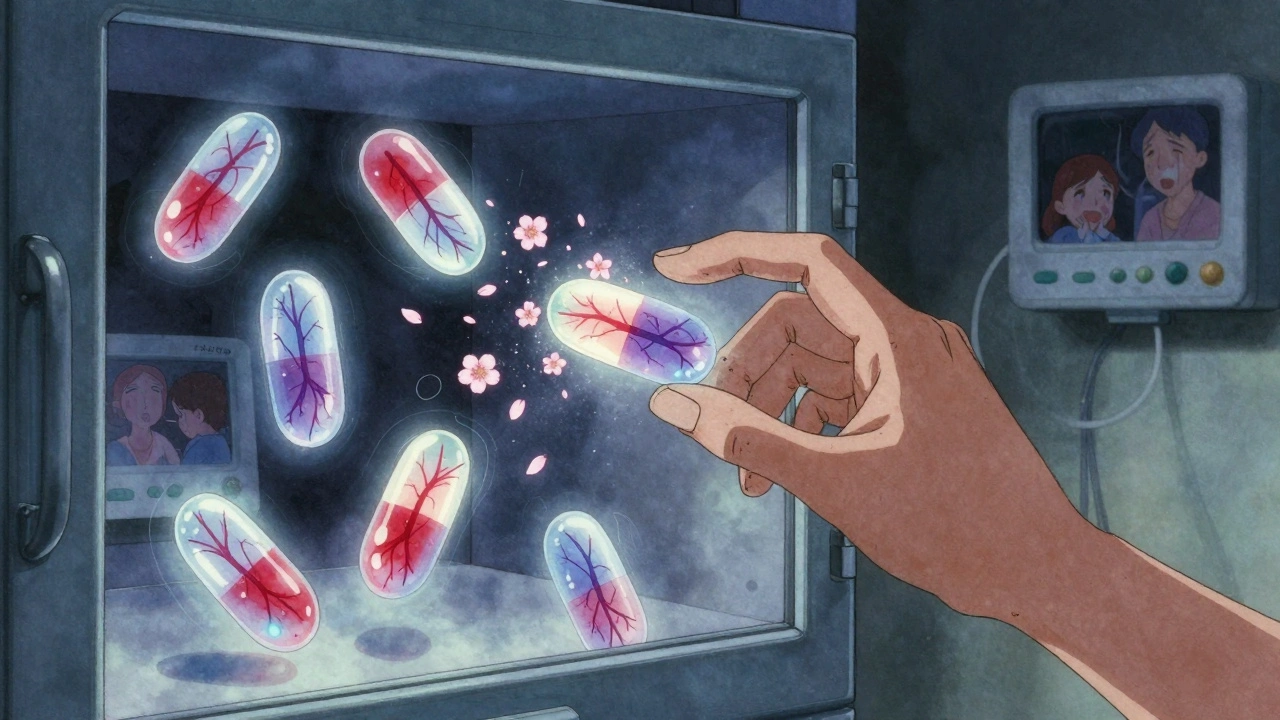
What Happens When You Take an Expired NTI Drug?
There’s no single story. The outcome depends on the drug, the person, and how much degradation occurred. But here are real-world scenarios:- A 68-year-old woman on warfarin after a mechanical heart valve replacement takes leftover pills from last year. Her INR drops from 2.8 to 1.6. She develops a blood clot in her leg. By the time she’s hospitalized, it’s traveled to her lung. She survives, but barely.
- A teenager with epilepsy switches from a new prescription of phenytoin to an old bottle found in her mom’s medicine cabinet. Her seizure frequency doubles. She ends up in the ER with status epilepticus.
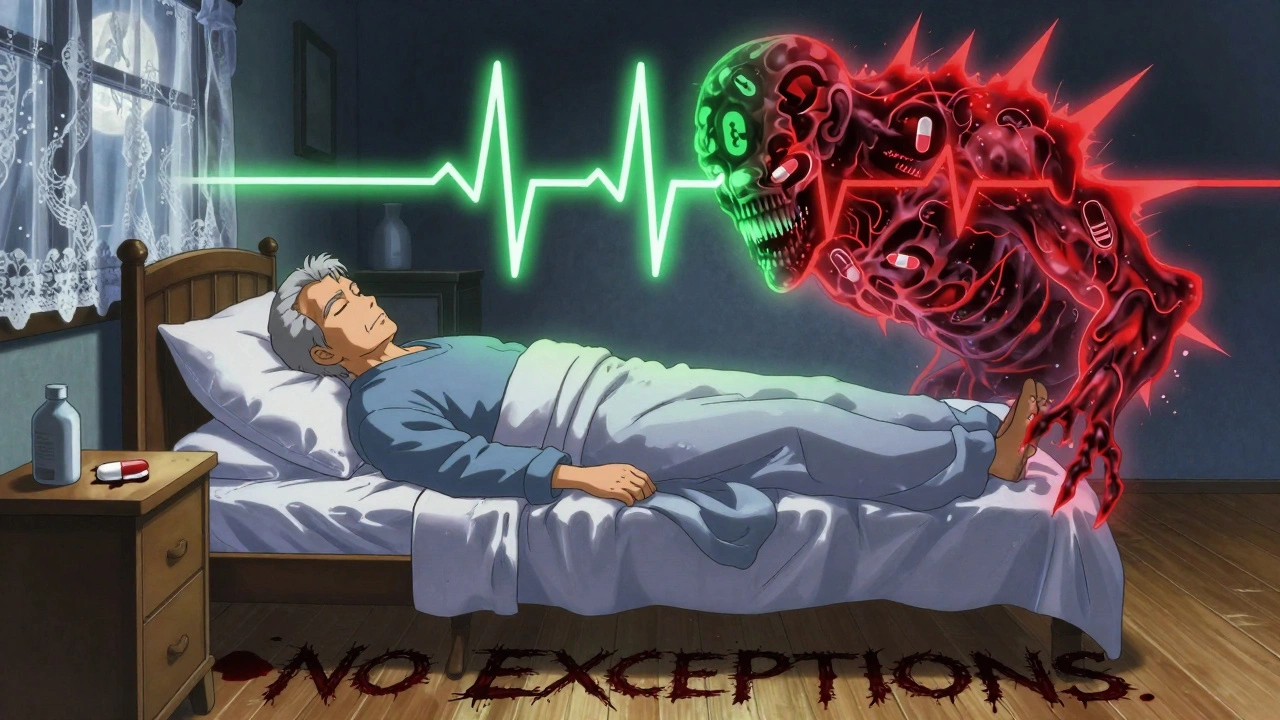
- An elderly man on digoxin for heart failure uses expired tablets because his insurance won’t cover the new refill. His blood level rises slightly due to inconsistent absorption from degraded formulation. He develops nausea, confusion, and a dangerous heart rhythm. He dies two days later.
How to Protect Yourself
If you or someone you care for takes an NTI drug, here’s what you need to do:- Never use expired NTI medications. Even if they look fine. Even if they’re only a month past the date. This isn’t a suggestion-it’s a safety rule.
- Ask your pharmacist to label NTI drugs clearly. Many pharmacies don’t. Request a sticker that says “Narrow Therapeutic Index-Do Not Use After Expiration.”
- Keep a current list of all NTI drugs you take. Share it with every doctor, ER, and pharmacist you see. Include the name, dose, and why you take it.
- Don’t switch brands or generics without consulting your provider. Even if the label says “equivalent,” NTI drugs aren’t interchangeable like aspirin.
- Store them properly. Keep them in a cool, dry place-not the bathroom, not the car. Heat and moisture speed up degradation.
- Dispose of expired NTI meds properly. Don’t flush them. Don’t toss them in the trash. Use a drug take-back program. Many pharmacies offer free disposal.
What Providers Should Do
Doctors, nurses, and pharmacists are on the front lines. Here’s what they need to do:- Treat all NTI drugs as high-alert medications. The Institute for Safe Medication Practices says so. That means double-checking doses, verifying prescriptions, and confirming patient understanding.
- Ask patients directly: “Are you using any medications past their expiration date?” Don’t assume they know the risk.
- Use therapeutic drug monitoring (TDM) when possible. Blood tests for lithium, digoxin, or phenytoin levels can catch problems before they become emergencies.
- Advocate for clearer labeling on NTI drug packaging. The American Pharmacists Association has called for this. It’s time it happens.
Bottom Line: Don’t Gamble With Your Life
Medications with a narrow therapeutic index aren’t like vitamins or antacids. They’re precision tools. A slight misstep, and things go wrong-fast. Expired pills might seem harmless. But for these drugs, they’re not. The FDA, the American College of Clinical Pharmacy, and the Institute for Safe Medication Practices all agree: when it comes to NTI drugs, expiration dates are absolute. There’s no gray area. No “it’s probably still good.” If you’re taking one of these drugs, your safety depends on consistency. Consistent dose. Consistent formulation. Consistent potency. And that means no expired pills. Ever.Can I still take an NTI drug if it’s only a week past its expiration date?
No. Even a few days past the expiration date can mean the drug has lost enough potency to become ineffective-or, in rare cases, cause unpredictable absorption. For NTI drugs like warfarin, lithium, or digoxin, there’s no safe buffer. The risk isn’t worth it.
Are all generic versions of NTI drugs unsafe?
No. Generic versions approved under the FDA’s stricter 90-111% bioequivalence standard are safe and effective-when they’re fresh and stored properly. The issue isn’t generics themselves, but using expired generics or switching between brands without monitoring.
How do I know if my medication has a narrow therapeutic index?
Check the prescribing information or ask your pharmacist. Common NTI drugs include warfarin, lithium, digoxin, phenytoin, levothyroxine, carbamazepine, and tacrolimus. If your doctor says you need regular blood tests to monitor your levels, you’re likely on an NTI drug.
What should I do if I accidentally took an expired NTI drug?
Call your doctor or pharmacist immediately. Don’t wait for symptoms. For drugs like warfarin or digoxin, even one missed dose or degraded pill can shift your blood levels. Your provider may need to run a blood test to check your levels and adjust your treatment.
Is it safe to use NTI drugs that are stored in the refrigerator after expiration?
No. Refrigeration slows degradation, but it doesn’t stop it. Expiration dates account for storage conditions. Even refrigerated NTI drugs should be discarded after the date. The risk of under- or overdosing remains too high.
Can I split NTI pills to save money?
Only if your provider approves it and the pill is specifically designed for splitting. Many NTI drugs, like levothyroxine, are not uniform in dose when split. A half-pill may not contain half the active ingredient. Never split NTI pills without professional guidance.


Queenie Chan
December 11, 2025 AT 08:41Wow. I never realized how delicate some meds are. I thought expiration dates were just corporate nonsense to make us buy more. But warfarin losing 10% potency and suddenly turning into a stroke risk? That’s terrifying. I just checked my cabinet - turns out I had an old bottle of levothyroxine from last winter. Tossed it. No questions asked. Thanks for the wake-up call.
Stephanie Maillet
December 12, 2025 AT 15:28It’s funny… we live in a world where we’ll meticulously track our sleep cycles, count our steps, and buy organic kale - but we’ll still swallow a pill that’s been sitting in a damp bathroom for 18 months, and call it ‘fine.’ We trust science when it’s convenient, and ignore it when it’s inconvenient. The body isn’t a vending machine; it’s a symphony. And NTI drugs? They’re the solo violinist. One wrong note… and the whole thing collapses.
Aileen Ferris
December 12, 2025 AT 23:54lol expiration dates are a scam. i took my grandmas digoxin that was 3 years out and she lived to 98. also, my cousin took expired insulin and still didn't die. the fda just wants you to buy more. also, i read on a forum that pills last forever if you keep em in the freezer. maybe we should all start storing our meds in the icebox?
Michaux Hyatt
December 14, 2025 AT 05:55Hey, thanks for writing this - seriously. I’m a pharmacist, and I see this all the time. People think ‘expired’ means ‘useless,’ not ‘dangerous.’ I’ve had patients bring in warfarin that’s 14 months past its date, shrug, and say, ‘It still looks fine.’ I always hand them a disposal bag and a free blood test coupon. If you’re on one of these meds, don’t guess - test. And if your pharmacy doesn’t offer free disposal? Ask them to start. We can do better.
Frank Nouwens
December 15, 2025 AT 09:12The scientific rigor behind expiration dating for narrow therapeutic index pharmaceuticals is both commendable and underappreciated. The pharmacokinetic variability introduced by degradation products, even at minimal levels, introduces a non-linear risk profile that is statistically significant in vulnerable populations. I would further recommend that healthcare institutions implement automated alerts in electronic health records when NTI medications are dispensed beyond their labeled expiration dates. This is not merely prudent - it is a bioethical imperative.
Nikki Smellie
December 16, 2025 AT 20:02Are you sure this isn’t a Big Pharma ploy? 😏 I mean, who really tests these expiration dates? And why do they always expire right before your insurance deductible resets? I’ve got a friend who works at a lab - she says the FDA just picks dates out of a hat. Also, my neighbor’s cat took expired lithium and lived. Coincidence? I think not. 🤔💊 #PharmaLies
Neelam Kumari
December 18, 2025 AT 19:11You people are so naive. You think expiration dates are the problem? Try living in India where 70% of meds are counterfeit. At least your expired pills are real - yours just don’t work. Meanwhile, my cousin’s uncle died from fake warfarin that looked exactly like the real thing. You’re worried about a few months past expiry? Focus on the real killers: corrupt supply chains, greedy doctors, and pharmacies that sell expired meds in slums. This post is a distraction.
David Palmer
December 19, 2025 AT 09:55lol i just took my dad's expired digoxin last week. he's been on it for 10 years. he's fine. i think this whole thing is overblown. also, why do you need to throw them away? just put 'em in a drawer. they don't go bad, they just get sleepy. also, i split my levothyroxine with a knife. works fine. stop being so scared of pills.