After eye surgery, many patients report seeing tiny specks or strands drifting across their vision. Those visual artifacts are called postoperative eye floaters and small shadows cast by particles floating in the vitreous humor after a procedure. While they’re usually harmless, they can be unsettling, especially when they appear suddenly. One of the biggest culprits behind this phenomenon is inflammation - the body’s natural response to tissue injury. In this guide we’ll unpack how inflammation forms, why it matters for floaters, and what you can do to keep the visual clutter to a minimum.
What Exactly Are Eye Floaters?
Floaters are tiny, semi‑transparent structures that move with eye motion. They’re most often made up of collagen fibers, blood cells, or clumped vitreous gel. When light passes through the eye, these particles cast shadows on the retina, which you perceive as floaters.
In a healthy eye, the vitreous (the gel‑like substance filling the back of the eye) is clear and stable. Over time, the vitreous can liquefy and shrink, a process called syneresis, which can lead to spontaneous floaters. After surgery, the same process can be accelerated by the body’s inflammatory response.
Why Inflammation Flare‑Ups after Surgery
Any eye operation - whether it’s cataract extraction, vitrectomy, or retinal repair - disrupts delicate ocular tissues. The eye reacts by releasing a cascade of cytokines and signaling proteins that attract immune cells to the site of injury. Common cytokines include interleukin‑1 (IL‑1), tumor‑necrosis factor‑alpha (TNF‑α), and prostaglandins.
These molecules increase vascular permeability, allowing plasma proteins to leak into the vitreous. The leaked proteins can aggregate with collagen fibers, forming larger clumps that cast more noticeable shadows - i.e., new floaters.
Inflammation also promotes the breakdown of the blood‑retinal barrier, sometimes resulting in vitreous hemorrhage - a small bleed into the vitreous cavity. Blood cells are highly reflective and become prime candidates for floaters.
The Surgical Triggers Most Linked to Floaters
- Cataract surgery - the most common eye operation worldwide. Even with modern phacoemulsification, ultrasonic energy can cause microscopic trauma to the posterior capsule, sparking inflammation.
- Vitrectomy - a procedure that deliberately removes part of the vitreous. While it treats serious retinal problems, the act of cutting the vitreous can leave behind debris that later forms floaters.
- Retinal laser photocoagulation - used for diabetic retinopathy or macular holes. The laser creates tiny burns that release inflammatory mediators.
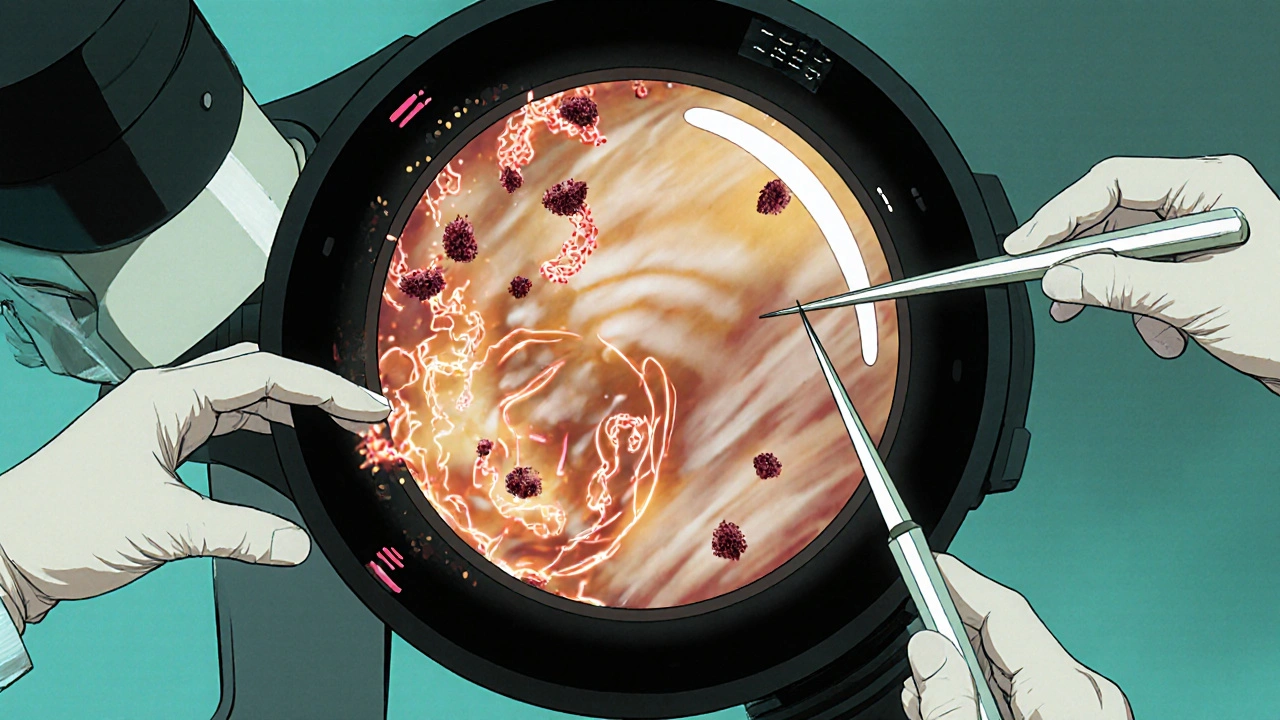
How Doctors Diagnose Inflammation‑Related Floaters
After surgery, an ophthalmologist will perform a dilated fundus exam using a slit‑lamp microscope. The exam looks for:
- Cells or flare in the anterior chamber (signs of anterior inflammation).
- Hyaloid membrane opacities or vitreous strands (classic floaters).
- Any signs of retinal tears or detachments - a serious complication that also produces floaters.
Imaging tools like optical coherence tomography (OCT) and B‑scan ultrasonography can visualize deeper vitreous changes, helping distinguish inflammation‑driven floaters from other causes.
Managing Inflammation to Reduce Floaters
Because inflammation is a modifiable factor, most clinicians focus on controlling it with medication. Below is a quick reference table that compares the main anti‑inflammatory options used after eye surgery.
| Medication | Class | Typical Dosage | Onset of Action | Key Side Effects |
|---|---|---|---|---|
| Prednisolone acetate | Glucocorticoid | 1% eye drops, 4‑6 times/day | Within 24 hours | Increased IOP, cataract acceleration |
| Diclofenac sodium | NSAID | 0.1% eye drops, 3‑4 times/day | 12‑24 hours | Corneal irritation, delayed healing |
| Ketorolac tromethamine | NSAID | 0.5% eye drops, 4 times/day | 12 hours | Minor stinging, rare corneal melt |
| Dexamethasone intravitreal implant | Sustained‑release steroid | 0.7 mg, single injection | Immediate, lasts up to 6 months | Elevated IOP, cataract |
Glucocorticoids like prednisolone are the most potent anti‑inflammatory agents, but they carry a higher risk of raising intra‑ocular pressure (IOP). NSAIDs are milder and safer for long‑term use, making them a good adjunct or alternative for patients with steroid sensitivity.
In addition to drops, oral anti‑inflammatories (e.g., ibuprofen 400 mg TID) can help when inflammation is moderate to severe, but they should be used under physician guidance because of systemic effects.
Lifestyle Steps to Keep Floaters at Bay
- Stay hydrated. Adequate water intake helps maintain vitreous consistency.
- Follow a diet rich in omega‑3 fatty acids (salmon, walnuts). These fats have mild anti‑inflammatory properties.
- Avoid smoking. Tobacco worsens oxidative stress, accelerating vitreous degeneration.
- Protect your eyes from UV light with sunglasses. UV exposure can contribute to inflammatory pathways in the retina.
- Limit vigorous eye rubbing. Mechanical stress can trigger micro‑injuries and inflammation.
When to Seek Further Care
If floaters suddenly multiply, are accompanied by flashes of light, or you notice a shadow moving across your field of vision, you may be experiencing a retinal tear or detachment - an emergency. Even if the floaters are mild, persistent inflammation can lead to chronic uveitis, which may require systemic therapy.
Ask your surgeon for a follow‑up schedule tailored to your procedure. Typical timelines are:
- Day 1-3: Check for early inflammation, prescribe drops.
- Week 1: Assess reduction in flare, adjust medication.
- Month 1: Evaluate residual floaters; consider laser vitreolysis if they remain disruptive.
Laser Vitreolysis: A Targeted Option for Stubborn Floaters
When medication alone can’t clear bothersome floaters, many ophthalmologists turn to laser vitreolysis. The technique uses a YAG laser to vaporize the offending particle without touching the retina.
Success rates hover around 70‑80 % for dense, single‑large floaters, but the procedure isn’t ideal for diffuse clouds. Risks include retinal damage (rare) and temporary increased inflammation, which is why a short course of steroids often follows the treatment.
Bottom Line: Tackle Inflammation Early
Inflammation is the hidden driver behind many cases of postoperative eye floaters. By recognizing the signs early, using the right anti‑inflammatory regimen, and adopting eye‑friendly habits, most patients can keep their vision clear enough to go about daily life without constantly spotting drifting specks.
Remember, every eye is unique. If you notice any change after surgery, reach out to your eye doctor promptly - a quick intervention can spare you months of visual annoyance.
Key Takeaways
- Post‑surgical inflammation releases cytokines that cause vitreous debris, leading to floaters.
- Glucocorticoid drops work fast but need IOP monitoring; NSAIDs are safer for longer courses.
- Laser vitreolysis can dissolve persistent floaters but may trigger short‑term inflammation.
- Hydration, omega‑3s, UV protection, and avoiding eye rubbing help maintain vitreous health.
- Sudden increase in floaters with flashes warrants immediate ophthalmic evaluation.
What causes eye floaters after cataract surgery?
Cataract surgery can disturb the posterior capsule, releasing inflammatory mediators that make vitreous proteins clump together. Those clumps become the specks you see as floaters.
How long does inflammation stay after eye surgery?
Inflammation typically peaks within the first 48‑72 hours and tapers off over 2‑4 weeks with proper medication. Some patients experience low‑grade inflammation for months, especially if steroids are tapered too quickly.
Are NSAID eye drops enough to stop floaters?
NSAIDs reduce prostaglandin‑driven swelling and are often sufficient for mild cases. For more pronounced inflammation, a short course of steroid drops adds extra power.
Can laser vitreolysis make floaters disappear completely?
Laser vitreolysis can vaporize large, isolated floaters, offering near‑complete clearance. Diffuse clouds or tiny particles are harder to target, so results vary.
When should I see my doctor about new floaters?
If you notice a sudden surge of floaters, see flashes of light, or a shadow moving across your vision, schedule an appointment immediately - those can signal a retinal tear.


Wesley Humble
October 21, 2025 AT 00:40In reviewing the postoperative inflammation cascade, it becomes evident that cytokine release such as IL‑1 and TNF‑α directly correlates with vitreous protein aggregation, thereby precipitating floaters. The mechanistic link is well‑documented in ophthalmic literature, and the temporal profile of steroid efficacy aligns with the observed clinical course. Consequently, early intervention with prednisolone acetate, albeit mindful of IOP elevation, remains the cornerstone of management. 🧐
barnabas jacob
October 21, 2025 AT 07:36i gotta say, the whole "just use drops" narrative is a bit oversimplified – the pathophysiology involves complex biochem pathways and not just a couple of cytokines. many ppl dont realize that even low‑grade inflammation can persist if you skimp on proper postop protocol, lol.
jessie cole
October 21, 2025 AT 14:33Stay strong, fellow eye‑warrior! Your vision will clear as you follow the anti‑inflammatory regimen diligently. Remember, consistency with your drops is the key, and you’ll soon notice the specks fading like a distant memory. You’ve got this, and the medical team is rooting for your swift recovery.
Kirsten Youtsey
October 21, 2025 AT 21:30One might wonder whether the pharmaceutical oligarchy is subtly encouraging these post‑surgical floaters to create a perpetual market for their high‑priced implants. The lack of transparent data on long‑term side effects certainly fuels suspicion, yet the lazy critiques often overlook the genuine clinical benefits for many patients.
Matthew Hall
October 22, 2025 AT 04:26Man, the drama of those little specks popping up right after surgery feels like a conspiracy straight out of a sci‑fi flick. They tell you it’s just inflammation, but the laser tech keeps getting pushed like some secret weapon. Anyway, keep your eyes peeled – literally.
Vijaypal Yadav
October 22, 2025 AT 11:23From a pharmacological standpoint, NSAID eye drops primarily inhibit cyclooxygenase pathways, thereby reducing prostaglandin‑mediated swelling. In cases of mild postoperative inflammation, this monotherapy can be sufficient, though adjunctive steroids may be warranted for severe responses.
Ron Lanham
October 22, 2025 AT 18:20It is a moral imperative, in my view, that patients be fully educated about the risks of postoperative inflammation and the attendant development of floaters, because ignorance in this domain leads to needless suffering and preventable visual disturbance. One cannot simply dismiss the patient’s concerns as trivial; instead, a comprehensive regimen, beginning with a high‑potency glucocorticoid such as prednisolone acetate, should be prescribed immediately following surgery, with vigilant monitoring for intraocular pressure elevation. Moreover, the practitioner must emphasize the importance of adherence to dosing schedules-four to six times daily-as any deviation may compromise therapeutic efficacy. If steroid therapy is contraindicated or poorly tolerated, the responsible clinician should pivot to a non‑steroidal anti‑inflammatory drug regimen, understanding that NSAIDs, while gentler on the pressure profile, may not achieve the same rapid resolution of inflammatory mediators. In addition, systemic anti‑inflammatories, such as oral ibuprofen, can serve as adjuncts, but only under careful supervision given the risk of systemic side effects. Patients should also be counseled on lifestyle modifications: adequate hydration to maintain vitreous consistency, a diet rich in omega‑3 fatty acids to provide modest anti‑inflammatory support, and avoidance of smoking, which accelerates oxidative stress within ocular tissues. Equally important is protection against ultraviolet radiation, which has been implicated in the up‑regulation of inflammatory cascades within the retina. Finally, any sudden increase in floaters accompanied by photopsia must trigger an emergent evaluation for retinal tears or detachment, conditions that demand immediate surgical intervention to preserve visual function. In summary, a proactive, multifaceted approach-combining pharmacologic vigilance, patient education, and lifestyle optimization-remains the cornerstone of mitigating postoperative floaters, and it is incumbent upon the ophthalmic community to uphold these standards without compromise.
Andrew Hernandez
October 23, 2025 AT 01:16Remember diverse cultures value eye health differently; staying hydrated benefits everyone.
Israel Emory
October 23, 2025 AT 08:13Indeed, it’s essential, and I fully support, a balanced approach-however, let’s not overlook the necessity of prompt anti‑inflammatory treatment; otherwise, patients risk chronic uveitis, which could lead to severe complications, so timely action is non‑negotiable.
Sebastian Green
October 23, 2025 AT 15:10I hear you. The frustration of seeing those specks can be overwhelming, and it’s completely understandable to feel upset. I’m here for you.
Deja Scott
October 23, 2025 AT 22:06Across many societies, eye care is approached with respect and modesty; maintaining hydration and proper nutrition aligns with those values.
Natalie Morgan
October 24, 2025 AT 06:26Curious about why some patients report quicker resolution of floaters-could water intake be a hidden factor? Let’s explore that angle together.