Pancreatitis Risk Assessment Tool
Understanding Your Risk
This tool helps you assess if your symptoms might indicate drug-induced pancreatitis. It is not a diagnostic tool, but it can help you determine if you should seek immediate medical attention.
Are You Taking High-Risk Medications?
Do You Have These Symptoms?
Most people assume pancreatitis only happens from drinking too much alcohol or having gallstones. But what if your prescription medication is the real culprit? Every year, thousands of people develop severe pancreatitis because of drugs they took without knowing the risk. It’s not rare. It’s not unusual. And if you’re on certain medications, you could be at risk right now.
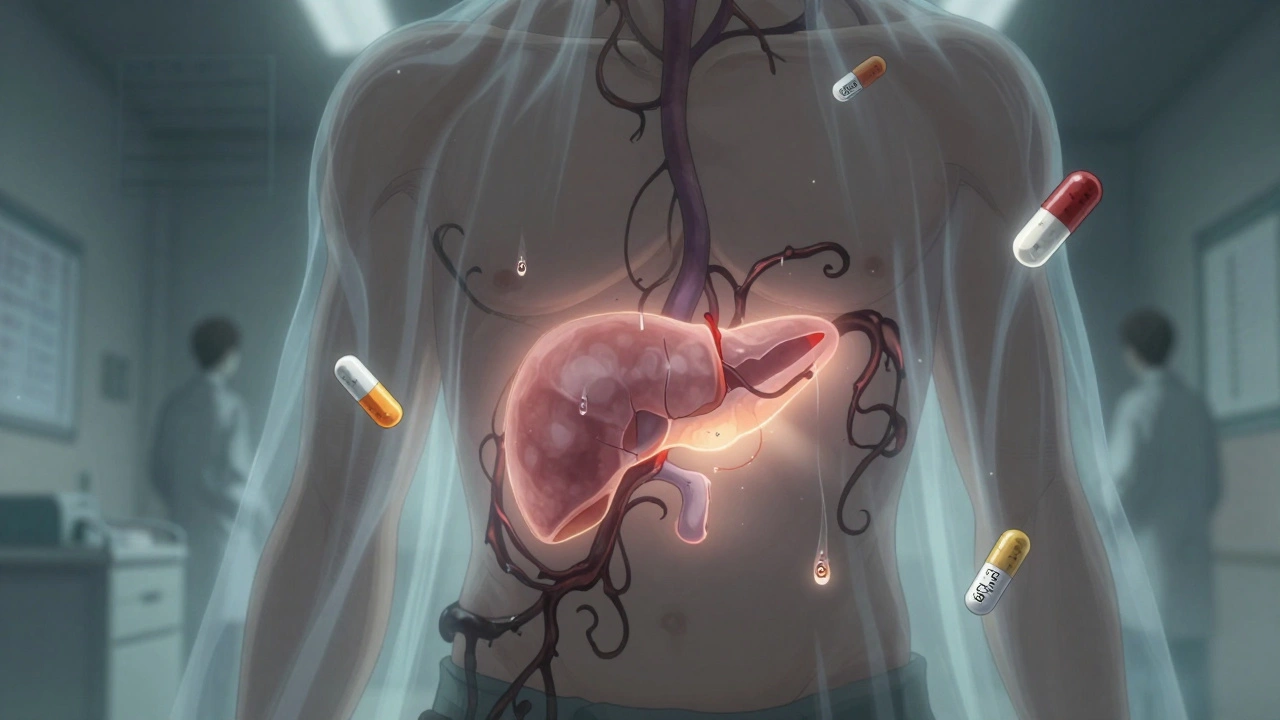
What Exactly Is Drug-Induced Severe Pancreatitis?
Severe pancreatitis from medications happens when a drug triggers dangerous inflammation in your pancreas - the organ behind your stomach that helps digest food and regulate blood sugar. In severe cases, parts of the pancreas die (necrosis), organs fail, and infections spread. Mortality rates hit 15-30%, higher than many gallstone-related cases. The good news? If caught early and the drug is stopped, your pancreas can heal completely.
This isn’t theoretical. In 2022, the FDA recorded over 4,200 pancreatitis cases linked to medications. The real number is likely higher because many cases go undiagnosed or mislabeled as stomach flu or acid reflux. The key difference? With drug-induced pancreatitis, symptoms don’t show up overnight. They creep in - days or even weeks after you start a new pill.
Which Medications Are Most Likely to Cause It?
Not every drug causes this. But eight classes carry strong, documented risk:
- ACE inhibitors - especially lisinopril and enalapril (commonly prescribed for high blood pressure)
- Diuretics - furosemide (Lasix) and hydrochlorothiazide
- Antidiabetic drugs - exenatide (Byetta), sitagliptin (Januvia), and newer SGLT2 inhibitors like dapagliflozin and canagliflozin
- Statins - simvastatin and atorvastatin (cholesterol-lowering pills)
- Immunosuppressants - azathioprine and 6-mercaptopurine (used for Crohn’s, lupus, rheumatoid arthritis)
- Anticonvulsants - valproic acid (used for seizures and bipolar disorder)
- Antiretrovirals - didanosine (rare now, but still in use in some regions)
- Oral contraceptives - especially older formulations with ethinyl estradiol
Valproic acid and azathioprine are especially dangerous. Studies show up to 22% of people taking valproic acid develop necrotizing pancreatitis - where tissue dies. For azathioprine, it’s around 18%. That’s not a small risk. It’s a red flag.
Warning Signs You Can’t Ignore
These aren’t vague symptoms. They’re sharp, specific, and often mistaken for something else:
- Constant, severe upper abdominal pain - feels like a knife or burning behind your ribs, often radiating straight to your back
- Pain that worsens after eating - especially fatty foods
- Nausea and vomiting - doesn’t go away with anti-nausea meds
- Fever above 38°C (100.4°F) - not just a chill
- Rapid heartbeat - over 90 beats per minute without exertion
- Swollen or tender abdomen - you can feel it when someone presses gently
One patient on Reddit described it: "I thought it was just bad heartburn. I took Tums for three days. Then I couldn’t breathe without crying. That’s when I went to the ER. My lipase was 2,800 - normal is under 60. They said if I’d waited another 12 hours, I might not have made it."
Another patient on Drugs.com shared: "I was on lisinopril for six months. One morning, I woke up with pain so bad I couldn’t stand. My doctor thought it was gastritis. I had to beg for a blood test. When they saw the numbers, they said, ‘You’re lucky you’re alive.’"
If you’re on any of the high-risk drugs above and you feel this kind of pain - don’t wait. Don’t assume it’s indigestion. Ask for a lipase blood test. Lipase is far more accurate than amylase for diagnosing pancreatitis. A level three times above normal confirms it.
Why Diagnosis Is So Hard - And Why It Matters
Doctors often miss drug-induced pancreatitis because it looks like every other kind. The pain mimics gallstones. The nausea feels like food poisoning. The timing is tricky - symptoms appear 7 to 14 days after starting the drug, sometimes longer. That makes it easy to blame something else.
One patient on HealthUnlocked wrote: "My rheumatologist told me my abdominal pain was just Crohn’s flaring. I was on azathioprine. By the time they did a CT scan, 40% of my pancreas was dead. I spent three weeks in the ICU."
That’s the danger. If you don’t connect the dots between your meds and your symptoms, you keep taking the drug - and your pancreas keeps dying.
The diagnostic criteria are clear: at least two of these three things must be true:
- Characteristic abdominal pain
- Lipase levels at least three times above normal
- Imaging (CT or ultrasound) showing pancreas inflammation or damage
And here’s the kicker: the only way to be 100% sure it’s drug-induced is to stop the medication - and see if you get better. No rechallenge (restarting the drug to test) is ever done because it’s too risky. So diagnosis is based on timing, exclusion of other causes, and improvement after stopping.
How It’s Treated - Step by Step
There’s no magic pill. Treatment is about support, timing, and stopping the trigger.
Step 1: Stop the drug immediately. This is non-negotiable. Delaying by more than 24 hours increases complication risk by 37%. If your doctor says, "Let’s wait and see," get a second opinion.
Step 2: IV fluids. You’ll get 250-500 mL per hour of saline through an IV. This keeps your pancreas perfused and prevents organ failure. Doctors monitor your hematocrit to make sure it stays between 35-44%.
Step 3: Pain control. Acetaminophen (Tylenol) is first-line. If that’s not enough, low-dose morphine is used - carefully. Avoid meperidine (Demerol); it can make things worse.
Step 4: Nutrition. You’ll be NPO (nothing by mouth) for the first 24-48 hours. But you won’t starve. If you can’t eat, a feeding tube is placed into your small intestine (nasojejunal) to deliver nutrients directly. The goal: 20-25 calories per kg of body weight by day three.
Step 5: Antibiotics? Only if there’s infection. Routine antibiotics do more harm than good. But if CT scans show infected necrosis, meropenem becomes standard.
Most patients improve within 7-10 days if the drug is stopped early. But if you wait, you could need surgery, ICU care, or even long-term enzyme replacement therapy.
Who’s at Highest Risk?
You’re not equally at risk. The data shows:
- Age 60+ - 68% of cases occur in older adults
- On five or more medications - average is 5.2 vs. 2.7 in non-drug cases
- On azathioprine, valproic acid, or SGLT2 inhibitors - highest mortality rates
- With kidney or liver disease - drugs stay in your system longer
And here’s something most people don’t know: your genes matter. If you’re taking azathioprine, a simple blood test can check for TPMT gene mutations. People with low TPMT activity have a 10x higher risk of pancreatitis. Testing before starting the drug can prevent disaster.

What You Can Do Right Now
Don’t wait for symptoms. If you’re on any of these drugs, take action:
- Write down every medication you take - including supplements and OTC pills.
- Check if any are on the high-risk list above.
- If you’re on one, ask your doctor: "Could this cause pancreatitis?"
- If you have new, unexplained upper abdominal pain - demand a lipase test.
- Keep a symptom journal: note when pain started, what you ate, and what meds you took.
One of the biggest mistakes? Patients assume their doctor knows all the risks. But doctors are overwhelmed. They may not remember that a 3-year-old statin prescription could suddenly trigger pancreatitis. You have to be your own advocate.
What’s Changing in 2025?
Things are getting better - slowly. The NIH launched the Drug-Induced Pancreatitis Registry (DIPR) in January 2023. It’s already tracked over 300 cases. The goal? Build a real-time map of which drugs cause what, and how fast.
Hospitals are now using automated alerts in electronic records. If you’re on lisinopril and your lipase spikes, the system flags it. In 78% of U.S. academic hospitals, this is already live.
And the FDA? They’re adding black box warnings to more drugs. In 2023, SGLT2 inhibitors got stronger labels after 87 cases in just 18 months. That’s a 4.3-fold jump.
But awareness still lags. Most primary care doctors still think of pancreatitis as an "alcohol problem." It’s time to change that.
Bottom Line: This Is Preventable
Severe pancreatitis from medication isn’t a fluke. It’s a warning sign you ignored. It’s a pill you didn’t question. It’s pain you thought would pass.
The truth? If you’re on a high-risk drug and you feel unusual abdominal pain - it’s not your imagination. It’s your body screaming. Stop the drug. Get tested. Save your pancreas. You won’t regret it.
Can over-the-counter drugs cause pancreatitis?
Yes. While most cases come from prescription drugs, some OTC medications can trigger it. High doses of NSAIDs like ibuprofen or naproxen have been linked to rare cases. Herbal supplements like green tea extract, kava, and black cohosh also carry risk. Always check with your doctor before combining new supplements with existing meds.
How long does it take to recover from drug-induced pancreatitis?
Recovery depends on severity. Mild cases often resolve in 5-7 days after stopping the drug. Severe cases with necrosis or organ failure can take weeks to months. Most patients who stop the offending medication early see full recovery. A small percentage develop chronic pancreatitis or diabetes if the damage is extensive.
Is it safe to restart the medication after recovery?
No. Once you’ve had drug-induced pancreatitis from a specific medication, you should never take it again. Even if you feel fine, restarting it carries a high risk of recurrence - and the second episode is often worse. Your doctor will find a safer alternative.
Can pancreatitis from drugs be fatal?
Yes. Severe drug-induced pancreatitis has a mortality rate of 15-30%. Death usually results from multi-organ failure, infection, or uncontrolled inflammation. The risk is highest if diagnosis is delayed or if you continue taking the drug. Early recognition and stopping the medication reduce death risk dramatically.
What should I ask my doctor if I’m on a high-risk drug?
Ask: "Is this drug known to cause pancreatitis? What are the warning signs? Should I get a baseline lipase test? Are there safer alternatives?" If you’re on azathioprine or valproic acid, ask about TPMT genetic testing. Don’t accept vague answers. This is a life-threatening reaction - you deserve clear answers.

Donna Hammond
December 12, 2025 AT 08:39This is life-saving information. I’m a nurse, and I’ve seen too many patients dismissed for 'just indigestion' when their lipase was through the roof. If you’re on any of these meds and have unexplained abdominal pain, don’t wait. Demand the test. Your pancreas can’t scream forever.
Also, please share this with your older relatives. They’re the most at risk and least likely to question their prescriptions.
Richard Ayres
December 14, 2025 AT 04:23An excellent and meticulously researched piece. The clinical details are precise, and the emphasis on early diagnosis through lipase testing is critically important. This kind of public health education is exactly what’s needed to bridge the gap between medical knowledge and patient awareness. Thank you for taking the time to compile this with such care.
Sheldon Bird
December 15, 2025 AT 05:00Yessss!! This needs to be everywhere!! 😊
I had a cousin who went to the ER thinking it was a stomach bug. Turned out it was lisinopril. She was in the hospital for three weeks. Now she’s fine, but she’ll never take another ACE inhibitor. Please, if you’re on meds and something feels 'off'-listen to your body. It’s not just gas. It’s your pancreas crying for help.
Share this. Save someone.
Karen Mccullouch
December 16, 2025 AT 07:59Of course Big Pharma doesn’t want you to know this. They make billions off these drugs while people die in hospitals. They bury the data. They silence doctors. You think this is an accident? It’s profit-driven negligence. And your doctor? Probably got a kickback from the rep who pushed that statin on you. 😡
Don’t trust the system. Check your meds. Fight back.
#PharmaKills
Michael Gardner
December 17, 2025 AT 03:20Interesting. But how many of these cases are actually caused by the drug vs. coincidental? I’ve seen people blame every new pill for every ache. Correlation isn’t causation. And why is there no mention of dose dependency or duration? This feels like fearmongering with a side of cherry-picked stats.
Willie Onst
December 17, 2025 AT 17:50Man, this hit home. I’m from Texas, and my grandma’s on all of these meds-lisinopril, statin, metformin. She’s 72. I showed her this post and she said, 'Well, I’ve had this tummy ache for weeks…' We’re going to the doc tomorrow.
Thanks for writing this like a real human. Not like a textbook. We need more of this.
Ronan Lansbury
December 18, 2025 AT 13:35How convenient that this 'FDA registry' was launched right after the pharmaceutical lobbying bill passed in 2022. The DIPR is a performative gesture. Real transparency would involve mandatory genetic screening before prescribing and full disclosure of adverse event data. But no-this is PR, not science. The real culprit? The FDA’s revolving door with drug executives. You’re being played.
Jennifer Taylor
December 19, 2025 AT 17:41OMG I KNEW IT!! I’ve been telling everyone for years!! I got pancreatitis after taking OTC ibuprofen for my back pain and they told me it was 'stress'!! I was in ICU for 10 days!! My blood was like, 'HELLO??' AND THEN THEY GAVE ME MORE DRUGS!! 😭
Now I only take turmeric and cry into my chamomile tea. Also, I think the government is using these meds to control our gut bacteria. I’m not crazy. I’ve seen the videos.
WHO ELSE HAS THIS HAPPENED TO?? LET’S FORM A SUPPORT GROUP!! #PancreasWarrior #StopTheChemtrails
Shelby Ume
December 21, 2025 AT 09:13Thank you for this. I’m a clinical pharmacist and I’ve been trying to get this message out for years. Many prescribers don’t realize that even 'safe' drugs like hydrochlorothiazide can trigger this. We need standardized screening protocols. Patients should be given a printed handout listing high-risk medications and warning signs when they’re prescribed anything new.
And yes-lipase is the gold standard. Amylase is outdated. Please, stop using it.
Jade Hovet
December 23, 2025 AT 07:28YOOOOO I JUST SAW THIS AND MY HEART STOPPED 😱
I’ve been on Januvia for 2 years and I’ve had this weird belly pain since last month… I thought it was just from eating too much pizza 🍕
Just called my dr’s office-left a message. If they don’t call back by tomorrow, I’m going to urgent care. I’m not waiting. I’m not ignoring it.
THANK YOU FOR THIS. I’m sharing this with my whole family. 💪❤️
nithin Kuntumadugu
December 25, 2025 AT 03:16LOL u think this is new? In India we know this since 2010. Azathioprine? Valproic? Everyone knows it kills pancreas. But u westerners always wait till u in ICU to learn. Also, why u think FDA care? They get money from pharma. U r all sheep. 😒
My cousin died from this. No one listened. Now I only take ayurvedic. No pills. Only turmeric, ginger, and vibes.
Harriet Wollaston
December 26, 2025 AT 01:02I’m so glad someone finally wrote this clearly. My mom had this happen after starting a new blood pressure med. She thought it was heartburn for a week. By the time they tested her lipase, she was in critical condition.
She’s fine now, but she says she’ll never trust a doctor again without asking, 'Could this hurt me?'
You’re not being paranoid. You’re being smart. Keep speaking up.
Lauren Scrima
December 27, 2025 AT 19:19Wow. So you’re saying if I take a pill, and then feel pain, it’s the pill? Shocking. 🤯 Next you’ll tell me smoking causes lung cancer.
Just kidding. This is actually brilliant. I’m printing this and taping it to my medicine cabinet. My pharmacist is going to hate me. 😘
sharon soila
December 29, 2025 AT 06:15This is one of the most important posts I’ve ever read. I am a retired nurse and I have seen too many patients suffer needlessly because they were not told the truth about their medications. The pancreas is a silent organ until it is too late. Please, if you are on any of these drugs, do not wait for symptoms. Ask your doctor for a lipase test. It takes five minutes. It could save your life.
You are not being dramatic. You are being responsible.
Thank you for sharing this knowledge with such clarity and compassion.