HAS-BLED Bleeding Risk Calculator
This tool calculates your bleeding risk score based on the HAS-BLED criteria for patients taking anticoagulants. A score of 3 or higher indicates high risk when combining with SSRIs.
Combining SSRIs with anticoagulants is more common than you might think. Millions of people take SSRIs for depression or anxiety, and millions more take blood thinners like warfarin or rivaroxaban for atrial fibrillation, deep vein thrombosis, or after a stroke. When these two types of medications are used together, the risk of serious bleeding goes up - not by a little, but by 33%. That’s not theoretical. It’s backed by data from over 42,000 patients studied in 2024. And the biggest danger? The first 30 days after starting both drugs at the same time.
Why Do SSRIs Increase Bleeding Risk?
SSRIs don’t thin your blood the way warfarin or Eliquis do. Instead, they mess with your platelets - the tiny blood cells that help clots form. Platelets need serotonin to stick together and seal up a cut. SSRIs block the serotonin transporter on platelets, which means serotonin gets washed out of them. Without enough serotonin, platelets can’t do their job properly. Studies show this cuts platelet aggregation by 30-40%. That’s like having slightly less glue in your blood when you need it.This isn’t a side effect you can feel. You won’t notice your platelets slowing down. But if you get a cut, have surgery, or develop a stomach ulcer, your body can’t stop the bleeding as quickly. That’s why gastrointestinal bleeding makes up 58% of cases when SSRIs and anticoagulants are used together. Intracranial bleeds, while rarer, are more dangerous - they happen 28% more often with this combo.
It’s Not About Which SSRI You Take
You might think stronger SSRIs like paroxetine are riskier than weaker ones like escitalopram. That’s what doctors assumed for years. But the latest research says otherwise. In a 2024 study of over a million patients, paroxetine and escitalopram carried the exact same bleeding risk - both increased major bleeding by 33%. Even sertraline, the most commonly prescribed SSRI in this group, showed the same pattern.This flips the old belief that serotonin reuptake potency equals bleeding risk. The real issue isn’t how strong the SSRI is - it’s that any SSRI depletes platelet serotonin. That’s why switching from one SSRI to another won’t reduce your risk if you’re still on an SSRI. The mechanism is the same across the board.
Anticoagulant Type Matters - But Not as Much as You Think
Warfarin has been the go-to blood thinner for decades. But newer drugs like apixaban, rivaroxaban, and dabigatran (called DOACs) are now used in most new cases. When paired with SSRIs, DOACs appear slightly safer than warfarin - 22% increased bleeding risk versus 28%. But here’s the catch: that difference wasn’t statistically significant. In plain terms, it’s not enough to say one is clearly safer than the other.Warfarin has another problem: it’s finicky. Its effect changes with diet, other meds, and even your liver function. That means your INR (a blood test that measures clotting time) can swing unpredictably. Add an SSRI on top, and you’re stacking two sources of bleeding risk - one mechanical (platelets), one chemical (INR fluctuations). DOACs don’t need regular blood tests, but they still impair clotting. So while DOACs are easier to manage, they don’t eliminate the SSRI-related platelet risk.
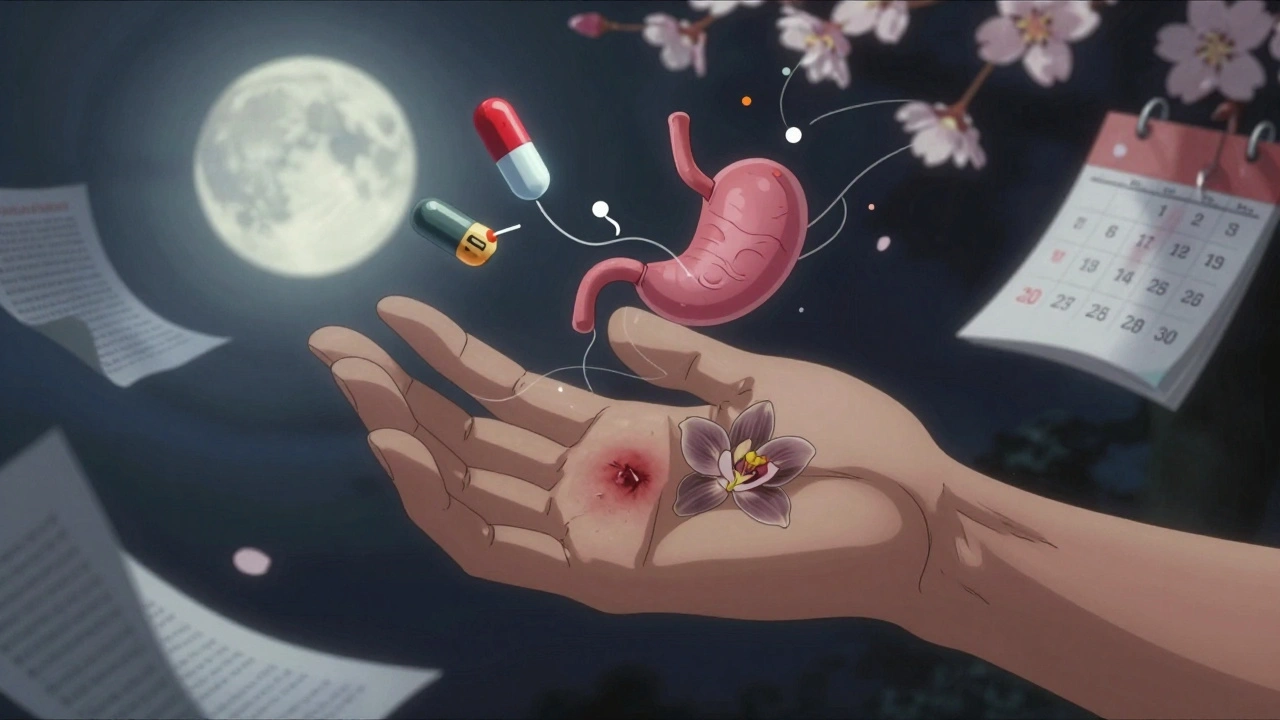
When Is the Risk Highest?
The first 30 days are the danger zone. That’s when the platelet serotonin levels drop fastest, and your body hasn’t adjusted yet. After six months, the risk drops back close to baseline. Why? Likely because your body adapts - maybe through new platelet production or changes in how serotonin is handled elsewhere.This timing matters for doctors and patients. If you’re starting an SSRI while already on a blood thinner, your doctor should watch you closely in those first weeks. Signs to look for: unusual bruising, nosebleeds that won’t stop, dark or tarry stools, or sudden headaches. If you’re on warfarin, your INR should be checked twice a week during the first month. For DOAC users, a baseline CBC and fecal occult blood test are recommended, with follow-ups every month for three months.
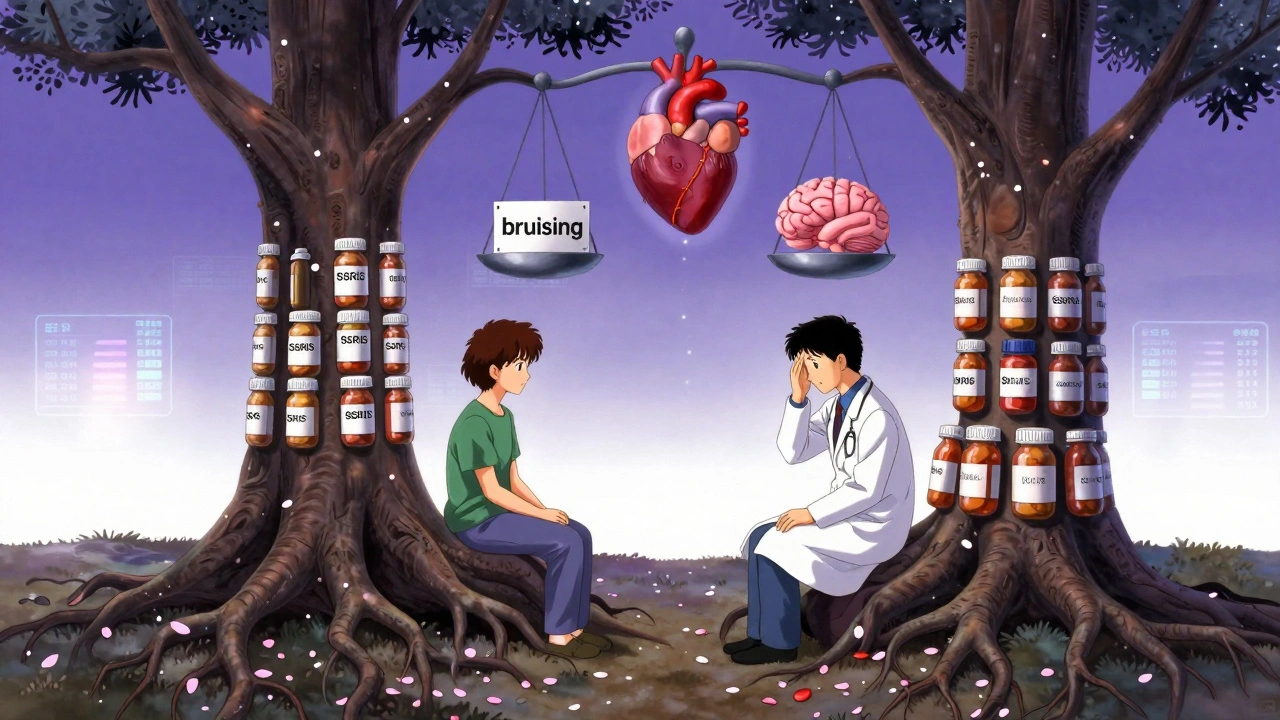
Who’s Most at Risk?
Not everyone on this combo will bleed. But some people are far more vulnerable. The HAS-BLED score is a tool doctors use to measure bleeding risk in people on anticoagulants. It looks at things like high blood pressure, kidney or liver disease, history of bleeding, and age over 65. If your score is 3 or higher, you’re in the high-risk group.For those patients, guidelines from the European Heart Rhythm Association and the American Psychiatric Association suggest considering non-SSRI antidepressants. Mirtazapine and bupropion don’t affect platelets the same way. They’re not perfect - mirtazapine can cause weight gain, and bupropion might raise seizure risk - but they’re safer options when bleeding risk is already elevated.
Still, SSRIs remain the first choice for moderate-to-severe depression in 87% of anticoagulated patients. Why? Because untreated depression is also dangerous. It raises the risk of heart attacks, stroke, and even death in people with heart disease. So the choice isn’t between “safe” and “risky.” It’s between “risky but treatable” and “untreated - and possibly deadly.”
What Should You Do?
If you’re on both an SSRI and an anticoagulant, don’t stop either without talking to your doctor. But do ask these questions:- Is my bleeding risk high based on my age, medical history, or other meds?
- Have I had any unexplained bruising or bleeding since starting the SSRI?
- Am I on warfarin or a DOAC? Does that change my monitoring plan?
- Is there a non-SSRI antidepressant that could work for me?
Primary care doctors prescribe this combo in 68% of cases where it’s inappropriate - meaning they didn’t fully weigh the risks. That’s why patient education is critical. If you’re on this combination, make sure you know the signs of bleeding. Keep a log of any unusual bruising, nosebleeds, or changes in stool color. Bring it to your next appointment.
What’s Changing in 2025?
The FDA updated anticoagulant medication guides in January 2025 to explicitly warn about SSRI interactions. They now recommend considering non-SSRI antidepressants in patients with additional bleeding risk factors. That’s a big shift - it’s no longer just a footnote in a drug label. It’s a formal recommendation.Meanwhile, the PRECISION-AF trial is underway. It’s tracking 5,000 patients on anticoagulants who are being randomly assigned to either an SSRI or a non-SSRI antidepressant. Results are due in late 2026. That study could finally tell us whether switching antidepressants reduces bleeding events - or if the risk is just too small to matter for most people.
The American College of Cardiology is also pushing for better clinical tools - software that can alert doctors when a patient on a blood thinner is being prescribed an SSRI, and suggest alternatives based on their bleeding risk score. This isn’t science fiction. It’s coming to electronic health records soon.


Brian Perry
December 2, 2025 AT 22:32so like… i took sertraline for 3 years and warfarin for my afib and never bled once… but my doc never told me about this so maybe i just got lucky??
Akash Sharma
December 3, 2025 AT 06:03okay but let’s be real-this whole thing is terrifying and also completely under-discussed. i’m 62, on rivaroxaban after a stent, and just started escitalopram last month because my anxiety hit like a truck. i didn’t know platelets needed serotonin to glue themselves together-that’s wild. i mean, it makes sense now that i think about it, but no one ever said it like that. i’ve had three nosebleeds in two weeks, thought it was dry air. now i’m paranoid every time i sneeze. also, why the hell do we still think SSRIs are all the same? if they all wreck platelets the same way, why do we keep prescribing them like they’re interchangeable candy? someone should make a flowchart. or a meme. i’d share it.
Michael Bene
December 4, 2025 AT 09:47oh sweet jesus this is why my uncle died in the ER with a GI bleed at 71. he was on citalopram and warfarin, no one told him to watch for dark stools, and his doctor just assumed he was ‘old and fragile.’ this isn’t a side effect-it’s a silent assassin. and now they’re pushing DOACs like they’re magic bullets? newsflash: they’re not. they just don’t need blood tests so docs don’t have to think. i’ve seen this play out too many times. if you’re on both, get a fecal occult blood test every month. no excuses. and if your doctor looks at you like you’re crazy for asking-find a new one. your life isn’t a spreadsheet.
Pooja Surnar
December 5, 2025 AT 13:12people just take meds like candy now. depression isn't an excuse to risk bleeding out. you should've tried therapy or yoga or something. this is why america is falling apart.
Sandridge Nelia
December 7, 2025 AT 03:42This is such an important post. I’m a nurse practitioner and I’ve seen this exact scenario-patients on SSRIs and DOACs, no monitoring, no education. I always screen for bruising and stool color during med reviews. I also tell patients: ‘If your poop looks like tar, don’t wait for your next appointment-go to urgent care.’ And yes, bupropion and mirtazapine are great alternatives when appropriate. We need more awareness, not just in docs’ offices but in pharmacy counseling too. 🙏
Mark Gallagher
December 8, 2025 AT 01:20Why are we letting foreign doctors dictate American medical practice? The FDA’s new guidelines are weak. We’ve had SSRIs for 30 years and Americans are still the healthiest people on earth. This bleeding risk is exaggerated by the pharmaceutical lobby to push expensive alternatives. Stick with what works. My grandfather took fluoxetine and coumadin for 15 years. He’s 94.
Pamela Mae Ibabao
December 9, 2025 AT 00:59So… you’re saying I can’t have my serotonin and my blood thinning too? 😔 I’m just trying to survive. I’m not asking for much. I just want to not cry in the shower and not die from a nosebleed. Is that too much? 🥲
Erik van Hees
December 10, 2025 AT 08:13Actually, the 33% increase is misleading. It’s a relative risk. Absolute risk? Still under 2% per year for most people. Most studies don’t even adjust for age, falls, or alcohol use. If you’re 28 and healthy, this is a non-issue. The fear-mongering here is worse than the risk. Also, if you’re on DOACs, your platelets aren’t the problem-it’s the anticoagulant itself. SSRIs are a footnote. Stop panicking.
Palanivelu Sivanathan
December 11, 2025 AT 06:53Think about it… serotonin is the soul’s glue, right? And SSRIs drain it from platelets like a spiritual leak… we’re not just altering biochemistry-we’re unraveling the metaphysical cohesion of human clotting. It’s poetic, really. The same molecule that lifts our mood also fails to seal our wounds. We are beings of paradox. The body remembers what the mind forgets. And yet… we still take the pills. Because the pain inside is louder than the blood outside. 🌀
Wendy Chiridza
December 13, 2025 AT 05:51I’m on sertraline and apixaban and had zero bleeding issues but I do get random bruises on my thighs. I thought it was from my dog jumping on me. Now I’m wondering… should I get a CBC? I’m 58, no other health issues, but I’m scared to ask my doctor because I don’t want to seem like a hypochondriac
Justin Hampton
December 14, 2025 AT 01:22Let’s be honest-this is just another way for Big Pharma to push more expensive drugs. Bupropion? Mirtazapine? Those are just rebranded SSRIs with different side effects. The real issue is that psychiatrists are lazy and don’t want to adjust doses. Stop blaming the meds. Start blaming the system.
Joanne Rencher
December 15, 2025 AT 23:25Wow. I’ve been on paroxetine and warfarin for 4 years. Never even thought to ask. My GP just handed me the scripts. I’ve had two nosebleeds last winter. Thought it was the heating. Now I feel stupid. And guilty. I’m not even sure if I should tell my doctor or just… stop one of them. 😣
Gerald Nauschnegg
December 17, 2025 AT 08:43Just had this exact conversation with my cardiologist yesterday. He said, ‘If you’re not bleeding, you’re fine.’ I said, ‘But what if I start bleeding and it’s too late?’ He paused. Then said, ‘I’ll refer you to a psychiatrist who knows this stuff.’ I cried in the parking lot. This isn’t just medical-it’s emotional. We’re supposed to trust our doctors. But no one tells us the real risks. I’m 39. I have a 5-year-old. I need to know what’s safe.
Cristy Magdalena
December 17, 2025 AT 10:46I’ve been on fluoxetine and rivaroxaban for 6 years. I’ve never bled. I’ve cried more than I’ve bled. So… what’s the real danger? The blood? Or the silence? I’m not stopping my meds. But I’m keeping a journal. Bruises. Stools. Moods. All of it. Because if no one else is going to track it… I will.
Siddharth Notani
December 19, 2025 AT 04:58Thank you for this detailed and scientifically accurate overview. As a medical researcher specializing in pharmacovigilance, I can confirm the 33% increased bleeding risk is robust and reproducible across multiple cohorts. The platelet serotonin depletion mechanism is well-documented in vitro and in vivo. Non-SSRI alternatives such as bupropion are indeed preferable in high HAS-BLED patients. I strongly encourage all clinicians to use clinical decision support tools as they become available. Stay informed, stay vigilant. 🙏