When we talk about obesity treatment, a medical approach to managing excess body fat that reduces health risks. Also known as weight management therapy, it’s not just about losing pounds—it’s about fixing the underlying metabolic, hormonal, and behavioral issues that keep weight off long-term. Many people think obesity is simply a lack of willpower, but science shows it’s a complex condition tied to genetics, environment, and chronic inflammation. Treatments that ignore this complexity often fail—and that’s why understanding your options matters.
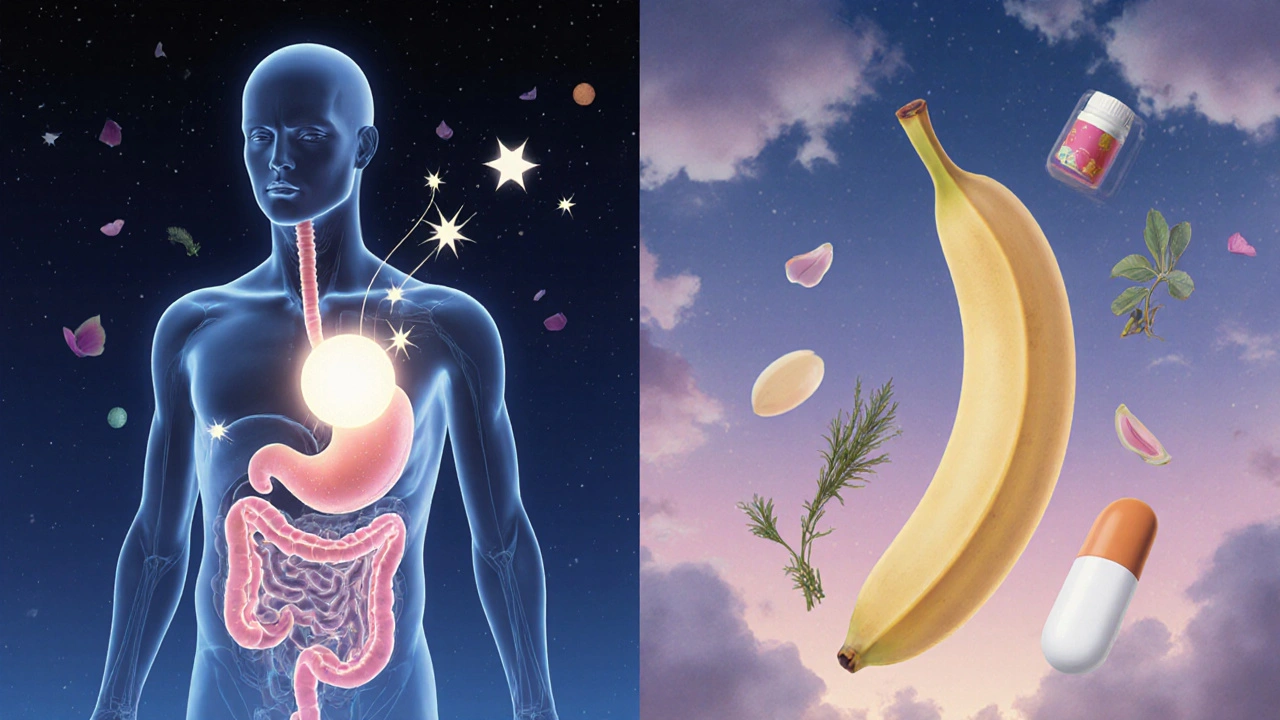
Effective obesity treatment, a medical approach to managing excess body fat that reduces health risks. Also known as weight management therapy, it’s not just about losing pounds—it’s about fixing the underlying metabolic, hormonal, and behavioral issues that keep weight off long-term. isn’t one-size-fits-all. For some, it starts with lifestyle changes for obesity, daily habits like improved nutrition, regular physical activity, and sleep hygiene that support sustainable weight loss. But for others, especially those with a BMI over 30 and related conditions like type 2 diabetes or high blood pressure, medication or surgery becomes necessary. Drugs like semaglutide and tirzepatide—originally developed for diabetes—have shown dramatic results in reducing body weight by targeting hunger signals in the brain. And for those with severe obesity, bariatric surgery, procedures like gastric bypass or sleeve gastrectomy that physically alter the digestive system to promote weight loss can lead to lasting remission of diabetes and heart disease risk.
What ties all these approaches together? They all address more than just calories in and out. They look at insulin resistance, gut hormones, stress, and even how your body defends its fat stores. That’s why simply eating less and exercising more often doesn’t work long-term—it ignores the biology behind the scale. The best outcomes come from combining approaches: medication to reset appetite, surgery to change digestion, and lifestyle support to maintain results. And it’s not just about looking different—it’s about feeling better, having more energy, and reducing your risk for heart disease, stroke, and certain cancers.
You’ll find posts here that dig into the real-world details: how to spot legitimate weight-loss meds, what side effects to watch for, how insurance covers bariatric procedures, and why some supplements claim to help but actually interfere with your treatment. Whether you’re just starting to explore options or already on medication and hitting roadblocks, this collection gives you the facts—not the fluff. No magic pills. No detox myths. Just clear, practical info on what works, what doesn’t, and how to navigate the system to get real results.