Understanding Inflammatory Bowel Disease
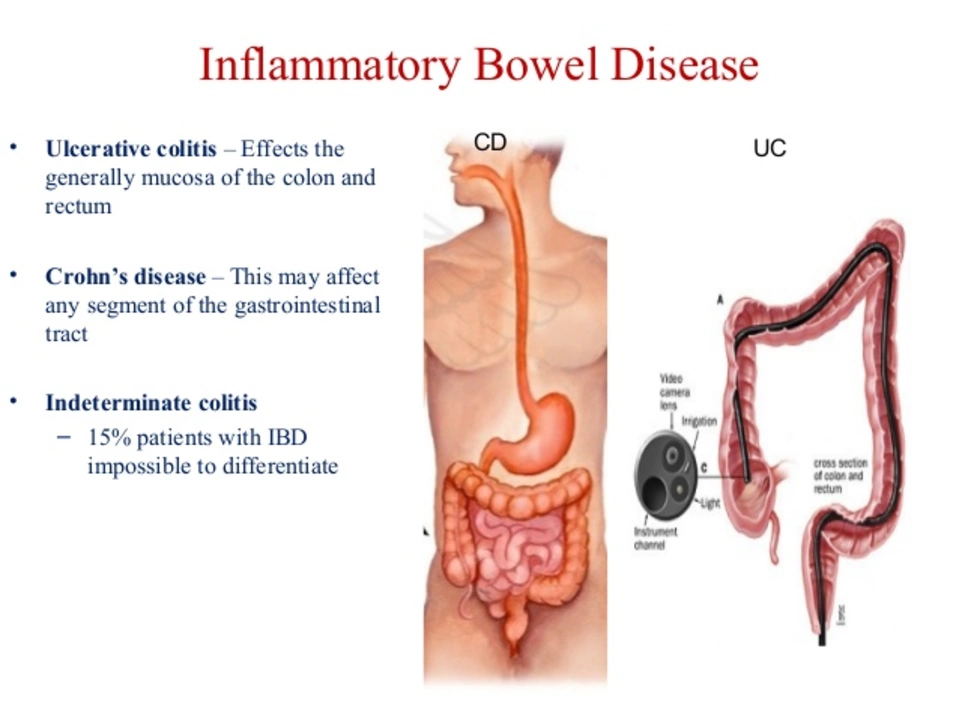
Inflammatory Bowel Disease (IBD) is a term used to describe chronic inflammatory conditions of the gastrointestinal tract, primarily Crohn's disease and ulcerative colitis. These conditions can cause a variety of symptoms, such as abdominal pain, diarrhea, weight loss, and fatigue. Living with IBD can be challenging, as the disease often has a significant impact on a person's quality of life. In this article, we will discuss the role of methylprednisolone in the management of IBD and the potential benefits it can provide for those living with these conditions.
Methylprednisolone: What is it and How Does it Work?
Methylprednisolone is a corticosteroid medication that is commonly prescribed to treat various inflammatory conditions, including IBD. Corticosteroids work by suppressing the immune system, which helps to reduce inflammation in the body. This can be particularly helpful for those with IBD, as the inflammation associated with these conditions is thought to be caused by an overactive immune response. By reducing inflammation, methylprednisolone can help to alleviate some of the symptoms associated with IBD and improve the overall quality of life for those living with these conditions.
Short-Term Relief: Using Methylprednisolone for Acute Flares
One of the primary uses of methylprednisolone in the treatment of IBD is for the management of acute flare-ups. During a flare, symptoms can become suddenly worse and require immediate intervention to bring the inflammation back under control. Methylprednisolone can be prescribed in high doses for a short period of time, typically ranging from a few days to a few weeks, to help rapidly reduce inflammation and alleviate symptoms. Once the flare has been brought under control, the dose of methylprednisolone is usually tapered down gradually to minimize the risk of side effects and avoid a rebound in inflammation.
Maintenance Therapy: Long-Term Use of Methylprednisolone
While methylprednisolone can be effective in the short-term management of IBD, it is generally not recommended for long-term use due to the potential for side effects. However, in some cases, a low dose of methylprednisolone may be prescribed as part of a maintenance therapy regimen to help control inflammation and prevent future flares. This approach is typically reserved for those who have not responded well to other treatments or who cannot tolerate other medications. It is important to carefully weigh the potential benefits and risks of long-term methylprednisolone use in consultation with a healthcare provider.
Important Precautions and Potential Side Effects
As with any medication, it is important to be aware of the potential side effects and precautions associated with methylprednisolone use. Some common side effects include weight gain, increased appetite, mood changes, and difficulty sleeping. Long-term use of methylprednisolone can also lead to more serious side effects, such as an increased risk of infections, decreased bone density, and elevated blood sugar levels. It is essential to discuss these risks with your healthcare provider and to closely monitor your health while taking methylprednisolone.
Alternatives to Methylprednisolone for IBD Management
While methylprednisolone can be an effective treatment option for some individuals with IBD, it may not be suitable for everyone. In some cases, alternative medications may be recommended to help manage inflammation and symptoms. These can include other corticosteroids, such as prednisone or budesonide, as well as non-corticosteroid medications like 5-aminosalicylates, immunosuppressants, and biologic therapies. It is important to work closely with your healthcare provider to determine the most appropriate treatment plan for your specific needs and circumstances.
Lifestyle Modifications and Complementary Therapies
In addition to medication, making certain lifestyle changes can also help to improve the management of IBD. This can include adopting a healthy diet, engaging in regular physical activity, and finding effective ways to manage stress. Some individuals with IBD also find relief from symptoms through complementary therapies, such as acupuncture, massage, or herbal supplements. It is important to discuss any lifestyle modifications or complementary therapies with your healthcare provider to ensure they are safe and appropriate for your specific needs.
Working with Your Healthcare Team to Optimize IBD Management
Ultimately, the goal of IBD management is to reduce inflammation, control symptoms, and improve overall quality of life. Methylprednisolone can play an important role in achieving these goals for some individuals, but it is essential to work closely with your healthcare team to develop a comprehensive treatment plan that is tailored to your specific needs. By staying informed about your condition and your treatment options, you can take an active role in managing your IBD and achieving the best possible outcome.

VEER Design
May 6, 2023 AT 21:02methylprednisolone? man, i remember when i was in the hospital for a flare-up and they gave me this stuff like it was candy. tasted like burnt sugar and made me feel like a superhero... until the moonface kicked in. 😅
Leslie Ezelle
May 7, 2023 AT 05:51THIS IS WHY PEOPLE DIE FROM LONG-TERM STEROIDS. NO ONE TELLS YOU ABOUT THE BONE LOSS. I LOST MY HIP TO OSTEONECROSIS BECAUSE SOME DOCTOR THOUGHT ‘JUST KEEP TAPERING’ WAS ENOUGH. #STEROIDSCANDAL
Dilip p
May 7, 2023 AT 06:56While methylprednisolone does suppress inflammation effectively, it’s crucial to understand that it doesn’t address the root cause of IBD-dysbiosis, epithelial barrier dysfunction, and immune dysregulation. It’s a band-aid, not a cure. Many patients develop steroid dependence because alternatives aren’t explored early enough.
Kathleen Root-Bunten
May 9, 2023 AT 02:48I’ve been on budesonide for 3 years now and honestly? Way better than methylprednisolone. Less weight gain, less mood swings, and I can actually sleep at night. My gastro said it’s because it’s targeted to the gut-less systemic impact. Just a thought for anyone stuck on the high-dose cycle.
Vivian Chan
May 11, 2023 AT 00:29Did you know the pharmaceutical companies funded 87% of the studies on methylprednisolone? They don’t want you to know about the herbal alternatives-curcumin, boswellia, even low-dose naltrexone. The FDA won’t approve them because they can’t be patented. This isn’t medicine-it’s a business model.
andrew garcia
May 12, 2023 AT 10:37Hey everyone, just wanted to say I’ve been on methylprednisolone for 6 months now and it’s been a rollercoaster. I’ve gained 20 lbs, cried at commercials, and slept like a rock. But I can eat again. And that’s worth something. 🙏
ANTHONY MOORE
May 13, 2023 AT 07:12Real talk: if you’re on this stuff long-term, you gotta move. Even if it’s just walking around the block. I did yoga every morning and it kept my bones from turning to dust. Also, drink water. Like, a lot. Your kidneys will thank you.
Jason Kondrath
May 14, 2023 AT 06:06Of course methylprednisolone works-it’s a nuclear option. But anyone prescribing it for maintenance clearly hasn’t read the 2023 ACG guidelines. This isn’t treatment; it’s medical laziness. I’ve seen patients become dependent on it because their doctors didn’t bother with biologics. Pathetic.
Jose Lamont
May 15, 2023 AT 16:01There’s something deeply human about how we treat chronic illness. We reach for the fast fix-the steroid, the opioid, the magic pill-because we’re terrified of the long haul. But healing isn’t about silencing symptoms. It’s about listening to your body, even when it screams. Methylprednisolone quiets the scream. But the wound’s still there.
Ruth Gopen
May 16, 2023 AT 03:11As a nurse who’s administered this drug for over 15 years, I’ve seen the side effects. I’ve held patients as they cried because they couldn’t recognize themselves in the mirror. I’ve watched their children grow up afraid to hug them. This isn’t just a medication-it’s a trauma. And we need to stop normalizing it.
Nick Bercel
May 17, 2023 AT 18:28Just a heads-up: if you’re tapering, DO NOT skip doses. I did. Got a flare back in 72 hours. Like, nuclear-grade. Now I set alarms. And I cry. A lot. But I’m alive. So… yeah.
Alex Hughes
May 18, 2023 AT 09:01It’s interesting how we treat corticosteroids as a monolithic solution when in reality their pharmacokinetics vary dramatically between individuals based on liver metabolism, gut microbiome composition, and even circadian rhythm-studies from the Mayo Clinic in 2021 showed that patients who took their dose at 8 AM had 37% fewer adrenal suppression events than those who took it at midnight, suggesting timing might be as important as dosage, yet this is rarely discussed in clinical practice, and even more rarely incorporated into patient education materials which tend to focus on generic warnings rather than personalized strategies
Hubert vélo
May 18, 2023 AT 18:11They’re using methylprednisolone to control symptoms so they can keep pushing you into colonoscopies and biopsies. It’s all a scheme. The real cure is detoxing from gluten, dairy, and EMFs. The FDA doesn’t want you to know that the gut is a bio-antenna. They profit from your dependence. I stopped the meds. I ate raw garlic. I’m symptom-free. They’re scared of what I know.
Kalidas Saha
May 20, 2023 AT 10:48Bro. I took methylprednisolone and my face looked like a balloon. My dog ran away. My girlfriend left. I cried for 3 days. Then I started meditating. Now I’m chill. And my gut? It’s like a zen garden. 🌿🙏