Every time you pick up a prescription, you’re handed a small piece of paper with a lot of words, numbers, and symbols. It might look like a cryptic code - and if you’ve ever stared at it confused, you’re not alone. But that label isn’t just paperwork. It’s your safety net. Each part of your prescription label is there for a reason: to make sure you get the right medicine, in the right amount, at the right time - and to keep you out of harm’s way.
Your Name - The First Line of Defense
Your name is printed at the top of every prescription label. It seems obvious, but this simple detail stops deadly mistakes. Every year, about 1.5 million medication errors happen in the U.S., and many of them occur because someone gets another person’s medicine. That’s why your name is front and center. If you see someone else’s name on the label, don’t take it. Even if the pill looks familiar, it could be the wrong dose or the wrong drug entirely. This one check has saved lives.
Medication Name - Brand vs. Generic
You’ll see two names here: the brand name (like Abstral is a brand name for fentanyl sublingual tablets) and the generic name (fentanyl is the active ingredient in Abstral). The brand name is what your doctor might say in the office. The generic name tells you exactly what chemical is working in your body. This matters because you might get the same medicine under a different brand later - or even a cheaper generic version. Knowing the generic name helps you recognize when you’re getting the same drug, no matter the packaging.
Dosage Strength - How Much Is in Each Pill?
This tells you how strong each pill, capsule, or milliliter of liquid is. For example: 100 micrograms per tablet of fentanyl. That number isn’t arbitrary. Too little might not work. Too much could be dangerous. If your doctor changes your dose, this number will change too. Always double-check it against what your doctor told you. If you’re unsure, call the pharmacy. Never guess.
Instructions - When and How to Take It
This is where most people get tripped up. It might say: "Take one tablet by mouth every 4 hours as needed for pain." Or: "Take with food." Or: "Do not crush." These aren’t suggestions - they’re rules. Some pills must be taken on an empty stomach or with water. Others can’t be chewed or split. Skipping instructions can reduce effectiveness or cause side effects. If you see abbreviations like "q.d." or "b.i.d.", ask your pharmacist. Most pharmacies now write them out in plain English: "once daily," "twice daily." But not all do.
Expiration Date - When It’s No Longer Safe
Every medication has a date after which it might not work as intended - or could even break down into something harmful. Most prescriptions expire 12 to 18 months after being filled. That doesn’t mean the pill turns bad overnight. But chemicals can change over time, especially if stored in heat or humidity. If you find an old bottle with an expired date, don’t take it. Throw it away properly. Many pharmacies offer take-back programs.
Prescription Number (Rx#) - Your Prescription’s ID
This number, often labeled "Rx#", is unique to your prescription. It helps the pharmacy track your refill history and verify your order. If you call in for a refill and the pharmacist asks for your Rx#, this is the number they need. It’s also how they make sure you’re not getting duplicate prescriptions from different doctors. If you switch pharmacies, you’ll need this number to transfer your prescription.
Pharmacy Info - Who Filled It and Who to Call
You’ll see the pharmacy’s name, address, and phone number. This isn’t just for show. If you have questions about side effects, interactions, or how to take it - call them. Pharmacists are trained to answer these questions. You’ll also see your prescriber’s name. That’s important if you need to contact your doctor about the medication. Keep this info handy. You might need it when traveling or if you’re seeing a new provider.
Visual Description - What the Medicine Looks Like
Many labels now include a short description: "White, round, film-coated tablet" describes the appearance of levothyroxine 50 mcg. This helps you confirm you got the right pill, especially if you’re taking multiple medications. If your pill looks different than last time - even if the label says the same thing - stop and call the pharmacy. Pills can look different if you switch brands or manufacturers. But if the shape, color, or imprint changes unexpectedly, it could be a mix-up.
National Drug Code (NDC) - The Medication’s Barcode
This 10- or 11-digit number is like a fingerprint for your medicine. It tells you exactly who made it, what the product is, and what size package it came in. Pharmacies and insurers use it to track prescriptions. You don’t need to memorize it, but if you’re ever asked for it - say by a pharmacist or insurance rep - you can find it printed on the label. The FDA has required this since 1987. It’s part of the system that helps prevent counterfeit drugs from entering the supply chain.
Storage Instructions - Keep It Safe
Some meds need to be kept cold. Others must stay dry. The label might say: "Store at 20°-25°C (68°-77°F)" is the standard room temperature range for most medications. If you keep your insulin in the bathroom cabinet, where steam and heat rise, it could lose potency. If you leave your liquid antibiotics on the windowsill, they might spoil. Always follow these instructions. A pill that doesn’t work because it was stored wrong is just as dangerous as one that’s expired.
Warning Labels - The Red Flags
These are the most important parts of your label. They might say: "May cause drowsiness", "Avoid alcohol", or "Not for use in pregnancy". These warnings come from real data - from clinical trials and real-world use. Ignoring them can lead to serious side effects. For example, mixing certain painkillers with alcohol can cause liver damage. Taking blood thinners with certain herbal supplements can cause dangerous bleeding. If you see a warning you don’t understand, ask your pharmacist. Don’t assume it’s not serious.
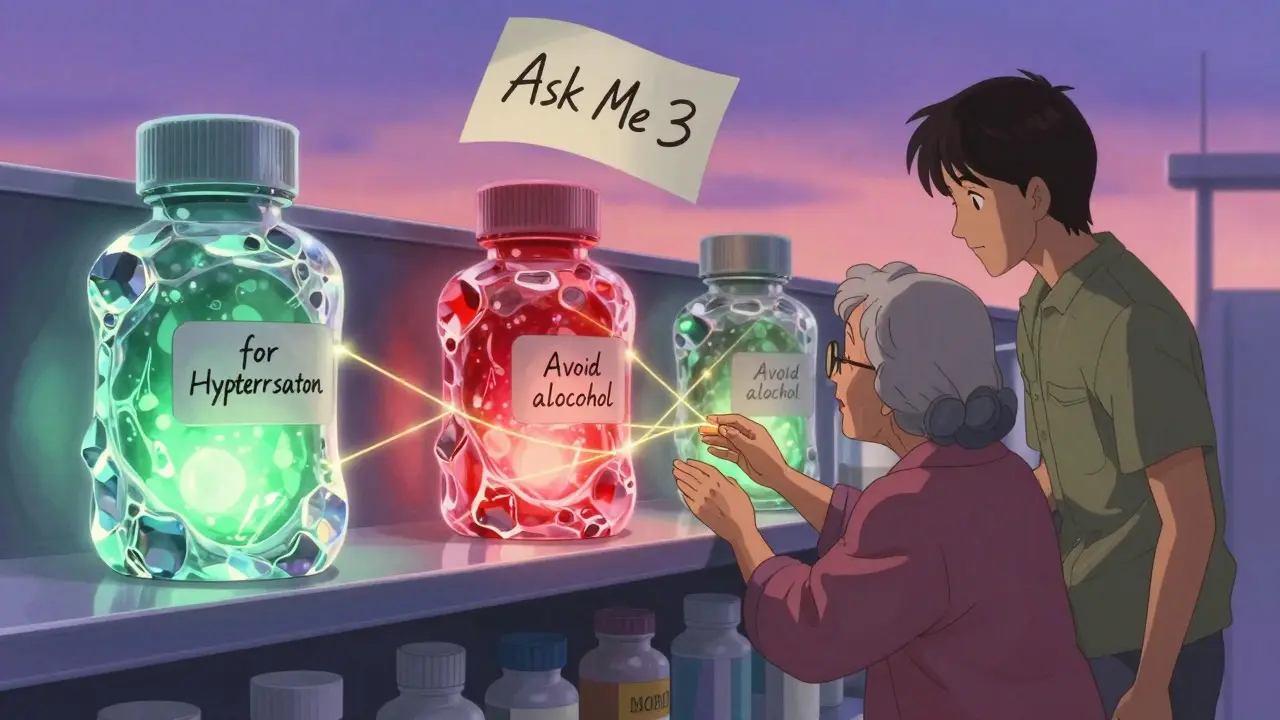
Why the Indication Matters - And Why It’s Missing
One of the biggest gaps in prescription labels? The reason you’re taking the medicine. Did your doctor prescribe this for high blood pressure? For anxiety? For infection? Many labels still don’t say. But including the indication - like "for hypertension" or "for migraines" - cuts wrong-medication errors by 55%, according to the Institute for Safe Medication Practices. A 2022 survey found that 62% of independent pharmacies still don’t include this, mostly because their electronic systems don’t support it. But if you ask for it, most pharmacists can print it out. And by 2025, the U.S. Pharmacopeia expects this to become standard across all prescriptions.
What You Should Do Every Time You Get a Prescription
Don’t just walk away with your meds. Take two minutes. Ask yourself these five questions:
- What is the name of this medicine - both brand and generic? Do I know why I’m taking it?
- What’s the dosage? Is it the same as last time? Did my doctor change it?
- How and when do I take it? With food? On an empty stomach? At night? Do I understand the instructions?
- What should I watch out for? Are there any warnings I need to follow? Any interactions with other meds I take?
- When does this expire? And where should I store it?
Use the "Ask Me 3" method too: What is my main problem? What do I need to do? Why is it important? If you can answer those three, you’re in a much better place.
What to Do If Something Doesn’t Look Right
If your pill looks different, the label has typos, or the instructions seem off - don’t take it. Call the pharmacy. Bring the bottle with you if you can. Pharmacists see these mistakes more often than you think. A misprinted label, a wrong dosage, or a mix-up with another patient’s prescription can happen. But catching it before you take it? That’s the whole point of the label.
How to Talk to Your Pharmacist
Pharmacists spend an average of 2.7 minutes counseling patients on new prescriptions. That’s not much - but you can make it count. Don’t be shy. Ask: "Can you explain this again?" or "Can you show me what this pill looks like?" Many pharmacies now offer pictograms - simple pictures showing how to take the medicine. Studies show those help people with low health literacy take their meds correctly 50% more often. If you’re a parent, ask for a dosing cup with clear markings. If you’re older, ask for large-print labels. Most pharmacies will give them to you.
The Future of Prescription Labels
Change is coming. Since 2020, 87% of new drugs approved by the FDA include patient-friendly labeling. That’s up from just 42% in 2016. By 2025, all new prescriptions will likely include the reason you’re taking the medicine. Some states are already testing labels with QR codes that link to video instructions. Others are adding color-coded strips for different dosing times. The goal? Make it impossible to mess up. Because right now, medication errors cause about 7,000 deaths a year in the U.S. That’s not just a statistic - it’s someone’s parent, sibling, or friend. Understanding your label isn’t just helpful. It’s lifesaving.
Why does my prescription label have two names for the same medicine?
The first name is the brand name, given by the company that made it. The second is the generic name - the actual chemical compound. For example, "Lipitor" is the brand, and "atorvastatin" is the generic. They’re the same drug. Generic versions are cheaper and just as safe. Knowing the generic name helps you recognize it if you switch pharmacies or get a refill from a different brand.
What if my pill looks different than last time?
If the shape, color, or imprint on the pill changed, call the pharmacy. It’s normal if you switched from brand to generic - manufacturers often change how pills look. But if the label says the same medicine and the pill looks totally different, it could be a mistake. Never take it without checking. Pharmacists can verify the medication using the NDC number on the label.
Can I take a medication past its expiration date?
Most medications lose potency after expiration, but few become dangerous. However, some - like insulin, liquid antibiotics, or nitroglycerin - can break down quickly and become ineffective or harmful. If you’re unsure, throw it out. Many pharmacies have drug take-back bins. Don’t flush it or toss it in the trash unless instructed. The FDA says: "When in doubt, throw it out."
Why doesn’t my label say why I’m taking this medicine?
Many labels still don’t include the reason - like "for high blood pressure" - because older pharmacy systems don’t support it. But this is changing. Studies show adding this detail reduces medication errors by over 50%. Ask your pharmacist to print it. By 2025, it will be required on all new prescriptions in the U.S. as part of updated USP standards.
What should I do if I miss a dose?
Check the label - it often says what to do. If it doesn’t, call your pharmacist. For most pills, if you miss a dose and it’s less than half the time until the next one, take it right away. If it’s been longer, skip it and wait for the next scheduled dose. Never double up unless told to. Overdosing can be dangerous. Always ask for clear instructions when you pick up a new prescription.